The FDA Approved The First CRISPR-Based Therapy. What’s Next?
17:26 minutes
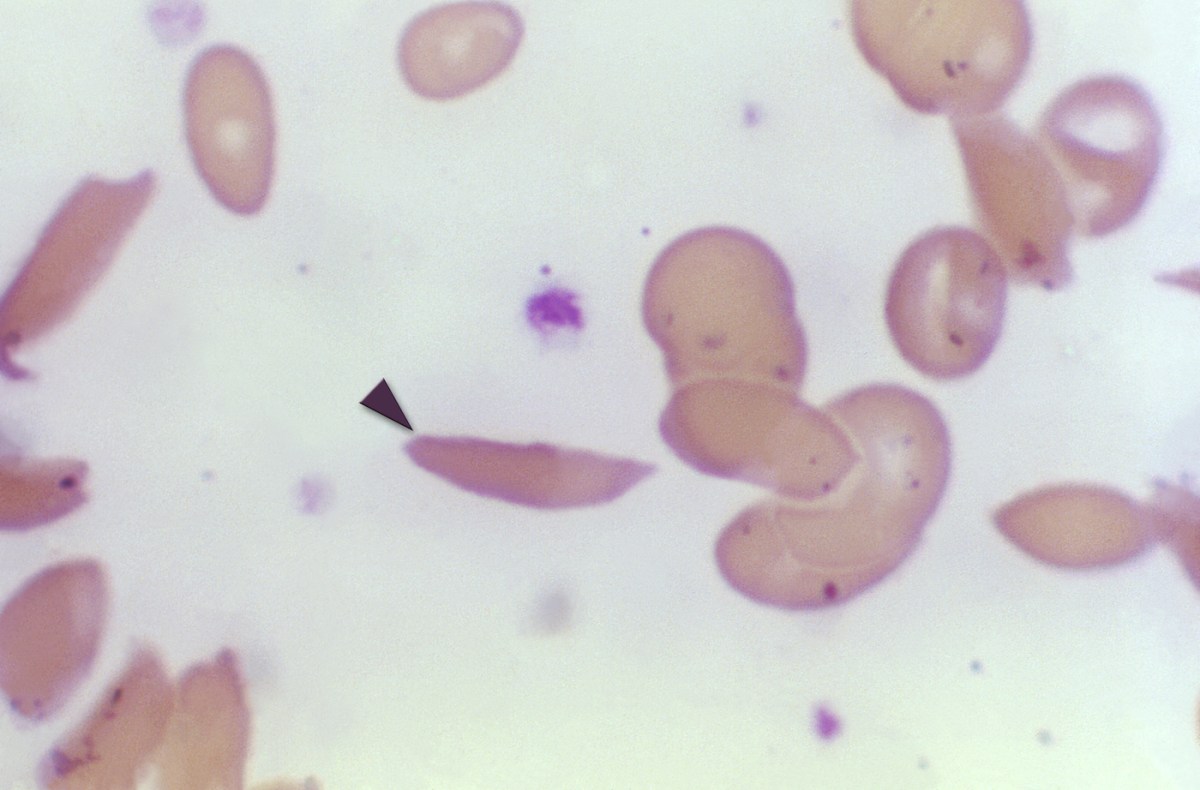
Last month the FDA approved a new treatment for sickle cell disease, the first medical therapy to use CRISPR gene editing technology. It works by identifying the gene or genes causing the disorder, modifying those genes and then returning them to the patient’s body.
There are now two gene therapies offered by pharmaceutical companies for sickle cell disease: Casgevy from Vertex Pharmaceuticals and CRISPR Therapeutics, and Lyfgenia from BlueBird Bio. But prices for these one-time treatments are steep: Casgevy costs $2.2 million per patient and Lyfgenia $3.1 million.
Both promise a full cure, which would be life-changing for patients with this debilitating condition. Over 100,000 Americans, mostly of African descent, have sickle cell disease.
This milestone raises more questions: What will be the next disease that CRISPR can help cure? And is it possible to reduce the costs of gene therapy treatments?
Ira talks with Dr. Fyodor Urnov, professor of molecular and cell biology and scientific director of technology and translation at the Innovative Genomics Institute, based at the University of California, Berkeley, about the future of CRISPR-based cures.
Conflict of Interest Disclosure: Dr. Fyodor Urnov is scientific co-founder, paid advisor, and holds equity in Tune Therapeutics. He is also a paid advisor for Ionis Pharmaceuticals and a paid advisor for Vertex Pharmaceuticals exa-cel program.
Fyodor Urnov is a professor in the Department of Molecular & Cell Biology and director of the Innovative Genomics Institute at the University of California, Berkeley in Berkeley, California.
IRA FLATOW: This is Science Friday. I’m Ira Flatow.
Last month, the FDA approved a new treatment for sickle cell disease, the first medical therapy to use CRISPR gene editing technology. Now it works by identifying the gene or the genes causing the disorder, modifying those genes, and returning them to the patient’s body. Two pharmaceutical companies are offering therapies using gene editing technology, and they promise a lifelong cure, which would be life changing for patients with this debilitating condition.
Over 100,000 Americans have sickle cell disease, most of whom are of African descent. Could this breakthrough herald a new era of CRISPR-based cures for genetic diseases? Given the astronomical prices for these new treatments, will they be affordable?
Joining me now to answer that question and more is my guest Dr. Fyodor Urnov, professor molecular and cell biology scientific director of technology and translation at the Innovative Genomics Institute. That’s at the University of California Berkeley. Welcome back to Science Friday.
FYODOR URNOV: Ira, what a joyful moment for me to join you again. Thank you for having me.
IRA FLATOW: You’re welcome. Thank you for joining us. For those of us who are not so familiar with CRISPR, what is CRISPR gene editing? How is it used to treat sickle cell?
FYODOR URNOV: Well, starting now you and I can call CRISPR as a tool that cures sickle cell disease. And that’s a remarkable statement. We’ve known about sickle for a very long time. We’ve known it’s caused by genes for 80 years. We’ve known its molecular cause since 1953. And here we are in 2024 where we can substantively say that dozens and dozens of folks in the United States and in Europe have had their life changed for the better because of this CRISPR thing. How does that work?
Well, we know what molecular circuit goes wrong when people get sickle cell disease. In fact, for a condition that’s so devastating for a human being living with it– there’s episodes of recurrent pain. There’s stroke. There’s damage to joints. The list is on and on and on.
The molecular causes on the surface level are quite simple. There’s hemoglobin that’s defective in one specific feature. CRISPR goes into the cells of a person with sickle cell disease and makes a tweak.
Now explaining what that tweak is takes a bit of time. In brief, what the CRISPR tweak does is allow mother nature to take out the equivalent of a spare tire out of her trunk if we think about normal hemoglobin as being the four wheels on a car and sickle hemoglobin as being these tires as defective. We have a different hemoglobin in our DNA. It’s called fetal. That word has many meanings, but in this particular case, it means a type of hemoglobin we make when we’re inside mom.
It turns out that if you flip that back on, sickle goes away. We’ve just never had a way to do that. CRISPR has shown up, and CRISPR in a number of folks has flipped that fetal hemoglobin back on. And there they are not experiencing pain, not having to do blood transfusions, not having to go to the emergency room. And as you mentioned, that’s right, the FDA and the MHRA in the United Kingdom have approved this as a medicine to treat sickle cell disease. Truly a remarkable moment.
IRA FLATOW: Let’s talk about why was sickle cell the candidate, the first disease, to get a CRISPR treatment?
FYODOR URNOV: There are several reasons. The benefit risk considerations are first and foremost. CRISPR is experimental technology. It was invented by Jennifer Doudna, my colleague here at UC Berkeley, and Emmanuelle Charpentier– they won the Nobel Prize for this in 2020– only 11 years ago. And to go in that period of time from an experiment done here on the UC Berkeley campus in a research lab to an approved medicine, that’s really fast. And so the benefit risk consideration is a human being living even in the best standard of care in the United States, their lifespan is shortened to just above 40 no matter how well we can treat that individual. And in Africa where the vast majority of folks with sickle live, the lifespan is typically about five years old. So it’s a terrible disease that deprives people of their ability to live a normal life. So for a new technology and experimental technology such as CRISPR, the benefit risk justification only works if you are approaching something that severe.
The second reason is it involves repairing of the blood, and here we’re actually standing on the shoulders of 60 years of physicians and physician scientists figuring out how to take blood stem cells out of the human body and then put them back in. This, of course, began with studies on bone marrow transplantation, for example, at the University of Washington where Don Thomas and team ultimately won the Nobel Prize for doing a bone marrow transplant, and there are thousands of them safely performed every year. In this case, the person becomes their own donor of bone marrow.
So you come into the hospital, your a blood stem cells are taken out your bone marrow, and then they’re CRISPR’d and then they’re put back in. So we can edit blood disease because we can take blood stem cells out, fix them, make sure that the repair has gone correctly, and then put them back in. Obviously, that’s going to be really hard for some other parts of the body like the liver or the heart or the brain.
And, you know, the third reason– and, look, I don’t want to be Negative Nancy, but I just want to be Nancy Realist. The third reason that it is a commercially viable target. You mentioned correctly that there are over 100,000 folks in the United States with sickle cell disease, and at least 20,000 of them are so sick with sickle that they really are eligible for this kind of treatment. And that means that a pharmaceutical company, which, of course, has a responsibility to return value to its shareholders, it makes sense for them to engage with sickle cell disease as a target because ultimately, let’s just be clear, these medicines are being developed and then provided in the context of a market economy.
And the reason I bring this up, Ira, is it’s not binarily celebratory moment for my field right now. In brief, yes, we have an approval for sickle. It’s joy all around, but there are hundreds of other blood diseases which could be repaired the same way that we do for sickle, and pretty much nobody in for-profit sector is working on them because there’s just not many folks with those diseases. And these companies are making the reasonable statement– reasonable for their business model. Why would we work on a disease that has 100 people?
These new medicines– and I should also point out that in addition to a CRISPR treatment for sickle– which was developed by Vertex Pharmaceuticals in collaboration with CRISPR Therapeutics. There is an additional genetic medicine for sickle now. It’s developed by a company called Bluebird Bio– it doesn’t involve CRISPR. It involves adding a gene, so it’s called gene therapy. So we now have two medicines, and the reason for that is there’s 20,000 folks in the United States just really eager to get that therapy.
IRA FLATOW: On the other hand, the cost of that, you mentioned it’s what we used to call an orphan disease. Drug companies weren’t going to make enough money on it to actually develop it, and you talked about these other diseases that are still out there yet even this medication, isn’t it priced at something like $2 million, $3 million a person?
FYODOR URNOV: Yes, it is.
IRA FLATOW: I ask rhetorically is that a price that any patient can afford?
FYODOR URNOV: Now that we have medicines that provide curative benefit for diseases as severe as sickle but also as prevalent as sickle, 20,000 people, it is the essential moment in the life of our field to ask how did we get to a situation where a cure for such a condition is that expensive, and what can we do critically moving forward to first of all make sure this medication is broadly available? And, second, how do we make future such medicines less expensive?
So in brief, part of the reason for the cost here is that it takes time to develop this. These pharmaceutical companies invested time and money in getting to the right solution. The other reason is it involves essentially bone marrow transplant, and the person is administered to the hospital and then is treated. And it’s not like they leave. They have to stay there in order to receive the medicine and recover from having received it.
I think strategically speaking, I really see ourselves as early in the lifespan of these genetic medicines. If you think of the first cures using genetic engineering– and those came to our field about 10 years ago– if you think of those as the moonshot, we landed on the moon, so now what? I think we as a community of scientists and physician scientists and regulators who develop these therapies have now even more motivation to ask ourselves 10 years from now how many more diseases will CRISPR have cured. And do we think that these medicines will still be priced at $2 million a person, or do we see a future where there will be a lot less expensive?
IRA FLATOW: And do we see a future where we will tackle those other orphan diseases that you mentioned no one’s– no one’s– no pharmaceutical company wants to tackle.
FYODOR URNOV: And obviously here I’m going to be a bright-eyed optimist. I think we absolutely will see a future where more and more of these diseases no matter what their prevalence is will be CRISPR tractable, and I am convinced that we will see a future where these are a lot more affordable. And why am I being so borderline Pollyannish here?
Well, first and foremost, we have never had a technology to treat disease like CRISPR. When Jennifer Doudna made her discovery here 11 years ago and published the paper in science, pretty much everyone working in the field at the time remembers that moment because all of us said there is no way this can be so simple. The way you take CRISPR and route it to repair a gene of interest uses rules that I can explain to my seven-year-old daughter. In fact, I have explained it to my seven-year-old daughter.
You take a gene of interest, you find a string of 20 letters, ACGT, you build a little nucleic acid that has a match to that string, you give it to Cas9, which is the core engine of CRISPR, and, bam, there’s the medicine. And, like I said, we’ve never had a technology that would be this frankly straightforward to design a first pass medicine with.
So because CRISPR is so conceptually straightforward to re-engineer for disease number 2 disease, number 3, disease number 384, this can only get faster. The very first human genome was sequenced over the course of about six years for $3 billion. Today, a human genome can be sequenced in three days for $1,000.
I think ultimately the way that larger companies will make money on CRISPR is by developing it to treat bigger disease indications. What I mean by that is cardiovascular disease, autoimmune disease, cancer, neurological disorder–
IRA FLATOW: Diabetes.
FYODOR URNOV: Diabetes, that’s right. And you’ll say to me but wait, Fyodor, come on. I thought those were not genetic. Well, they are, and they aren’t.
There is a company called Verve, and they’re building a medicine for a genetic form of heart disease. It’s a terrible disease. It’s, again, genes mutant, bad cholesterol, really bad cholesterol. So– but they are correctly reasoning that if they are successful in developing this medicine into something that works in familial cardiovascular disease that they’re going to be able to use it to treat sporadic cardiovascular disease such as affects tens of millions of people.
And they’re not being unrealistic in that expectation. Statins, which I know a lot of your audience takes, they were not developed initially to treat or even prevent sporadic cardiovascular disease. They were developed to treat genetic disease.
Once Big Pharma steps into the space and starts to commercialize CRISPR medicines of such size, I am hopeful that there will be abundant room to not forget about the genetic diseases. So first of all, people call them rare. They’re rare individually, yeah. Bubble boy disease. Everybody knows there’s like 50 people with bubble boy disease.
But collectively they affect about 300 million people on planet Earth. It’s just that the individual diseases are rare. My hope and certainly a major focus of our effort here at the Innovative Genomics Institute which Jennifer Doudna founded but also across the field, there’s a major effort in, quote, academic, unquote, science in the nonprofit sector to really build scalable treatments for genetic diseases. That’s our plan to go from the rare to larger disease populations.
IRA FLATOW: Listeners at home are going to be thinking I have a rare genetic disorder. My child does or someone in my family does. There’s not currently a treatment. What is a realistic timeline for when we might see more CRISPR-based therapies developed at a price people can afford?
FYODOR URNOV: The number one rule in my field is never give patients false hope. Everyone who works on CRISPR gene editing receives emails that don’t just break your heart. They shatter your heart. I got an email from a parent with a photograph, and the email started with, dear Dr. Urnov, can you save my dying angel. And you just– you have to stop and start crying and then get back together and see what you can do for this human being.
The reality is if we start today on a rare disease, it will take us three to four years to get to the clinic best case scenario. Why? Because we have to follow stringent rules for developing these experimental medicines. Then after that it will take a year or two, three, four longer to actually show that this is safe and effective and ultimately get Food and Drug Administration or European regulators approval.
So I want to be very cautious to not give your listeners false hope. Having said that, the federal government– I’m very proud to say that our country has invested– the federal government has invested in an all academic, all non-profit effort to build CRISPR cures for multiple diseases, and for probably the first time in our nation’s history, the feds are picking up the tab. Why are they doing that? For precisely the reason we just discussed.
The goal is not to treat and this program to be clear aims to only, quote unquote, treat 10 such diseases out of 5,000. Is that a lot? Well, not really. But the remit from the federal government is that we do this in a way where we could then do if you will control A, control C, control V. Namely we can copy paste everything we’ve learned about how to do CRISPR cure for a disease number 1 to do a crisper cure for a disease number 2. That’s a related genetic condition.
IRA FLATOW: You want a recipe. You want to create a recipe.
FYODOR URNOV: We want to create a codebook. We want to create a codebook. That’s exactly right. And so I really salute the federal government for having made this investment. Here in the state of California– very, very proud to be a professor at UC Berkeley– the California taxpayer has funded the California Institute for Regenerative Medicine, which is an entity which funds such CRISPR cures research across the state.
Now unfortunately California is the only state with this initiative. I think the path forward is to basically provide more federal and state support. At this moment in time, when– I’ll just give you a pretty stark number– the five leading biotech companies that have commercial rights to develop CRISPR– various flavors of CRISPR, I think together are working on like 10 diseases out of 5,000.
So now is the moment in time when I think more federal and state support and philanthropic support, you name it, is essential to not just keep the pilot light and the stove alight. No, no, no. To make sure that we have more metaphorically speaking irons in the fire. So if the next five or six years can feature such evidence for, pick a number, 10 to 20 such genetic diseases, I’m absolutely convinced that the five or 10 years beyond that will feature an exponential expansion of the imprint of positive footprint of CRISPR on health care.
IRA FLATOW: Dr. Urnov, I want to thank you for taking time to be with us today, and I wish you would come back and tell us more about some of your work as the progress is going.
FYODOR URNOV: Thank you very much for having me on the show for showcasing gene editing as a therapeutic modality and for reminding us all that the new technology that once could be in a lab at a research university can become a cure faster than we think.
IRA FLATOW: Dr. Fyodor Urnov, professor molecular and cell biology scientific director of technology and translation at the Innovative Genomics Institute that’s at UC Berkeley based, of course, in Berkeley, California.
Copyright © 2023 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Shoshannah Buxbaum is a producer for Science Friday. She’s particularly drawn to stories about health, psychology, and the environment. She’s a proud New Jersey native and will happily share her opinions on why the state is deserving of a little more love.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.