Living With Coronavirus, Behind Bars
29:44 minutes
 This segment is part of The State of Science, a series featuring science stories from public radio stations across the United States. Read four features about the state of COVID-19 in prisons from station reporters in Ohio, Arizona, Indiana, and California.
This segment is part of The State of Science, a series featuring science stories from public radio stations across the United States. Read four features about the state of COVID-19 in prisons from station reporters in Ohio, Arizona, Indiana, and California.
As the COVID-19 pandemic has spread, it’s become clear certain populations are particularly at risk—including those serving sentences in prisons and jails. The virus has torn through correctional and detention centers across the U.S., with more than 78,000 incarcerated people testing positive for COVID-19 as of July 28, according to the Marshall Project’s data report.
“Prisons are just the worst possible environment if we are trying to reduce infectious disease,” Zinzi Bailey told SciFri earlier this week on the phone. She is a social epidemiologist at the University of Miami and a principal investigator of the COVID Prison Project, which tracks and analyzes coronavirus data in U.S. correctional facilities. “A lot of people would argue that the conditions are inhumane.” Disease outbreaks have swept through prisons in the past, often due to poor living conditions and limited access to proper health care, Bailey explains. Hepatitis, tuberculosis, and HIV are just a few of the diseases that have historically hit inmates hard.
Now, the incarcerated, correctional officers, and staff members are battling COVID-19. Detention centers are notoriously overcrowded, making it easy for the virus to spread. The cramped, dormitory-style living conditions, shared spaces, and infrequent sanitation can contribute to increased risk of exposure and infection. In Ohio, for example, the prison system is at 130% capacity, making it “basically impossible” to socially distance inmates, Paige Pfleger, health reporter at WOSU in Columbus, Ohio, told SciFri on the phone last week.
“I got letters from all these inmates saying they were scared of dying.” — Jimmy Jenkins
Yet incarcerated people living in these conditions have little to no access to protection. Some have resorted to making face coverings out of shirts and boxer shorts. At the beginning of the pandemic, some correctional officers in Arizona prisons were not allowed to wear masks.
“Correctional officers were originally told that if they did wear masks, it would scare inmates—that they’re going to think, ‘Oh my gosh, this is a really serious virus,’” says Jimmy Jenkins, senior field correspondent and criminal justice reporter at KJZZ in Phoenix, Arizona. “I got letters from all these inmates saying they were scared of dying.”
Access to testing among the incarcerated population has also varied state to state. Ohio conducted mass tests in some of the facilities in April, but have been unable to retest in order to track community spread, says Pfleger. In Arizona, inmates are reporting that “only the sickest of the sick are actually getting tested,” says Jenkins.
“It’s like an experiment, and we are letting it run its course in these prisons.” — Zinzi Bailey
Coronavirus outbreaks in prisons often spill over into the rest of the community. Contract workers and correctional officers coming in and out of detention facilities can cause further spread of the virus. This is concerning, particularly in Black, Latino, and Native American communities with an already increased risk of contracting the disease.
“We believe that there’s going to be a connection between the communities of color that are around prisons, and the prisons themselves,” says John Eason, an assistant professor of sociology at the University of Wisconsin-Madison, who spoke to Science Friday over the phone earlier in the week. In an ongoing study with the Dane County Criminal Justice Council, “we’re going to be able to parse that out to see the role of corrections officers.” He suspects they may find officers are “basically incubators—or vectors between communities and the prisons that they work in.”
Invest in quality science journalism by making a donation to Science Friday.
Paige Pfleger and Jimmy Jenkins tell us more about how their states are responding to coronavirus outbreaks in prisons. Then, social epidemiologist Zinzi Bailey provides a closer look at the trends in American prisons—and what COVID-19 is revealing about public health in these systems.
Read more about the state of COVID among the incarcerated population, from local public radio reporters across the U.S.

Ohio has one of the oldest prison populations in the United States, largely due to charges stemming from the state’s war on drugs. A fifth of the population is over the age of 50—a group known to be more vulnerable to COVID-19. “People are out in the yard in wheelchairs and walkers. The prison population is just that old,” says Pfleger. “Those populations that hold a lot of the old prisoners are also the populations that have a lot of COVID cases, and specifically, a lot of COVID deaths.”
In April, Ohio was one of the first to roll out mass testing in detection facilities. At Marion Correctional Institution, the tests revealed more than 80% of the population was already infected. The state tried separating and moving people who tested negative from those who tested positive. However, inmates reported that they did not receive their test results when they were relocated.
“Nobody is saying nothing, they’re just leaving us up here,” Marion Correctional inmate Andre Stores told Pfleger in an WOSU article. “It’s like they’re leaving us to basically die. I didn’t come to prison to die.”

Employees working in a contracted food services group at Florence and Yuma state prisons tested positive for COVID-19, Jenkins reported on May 18. Later that week, an outbreak spread among inmates. At the time, correctional officers had to pay for their own tests, and were only required to self-report (as of May 21, officers were billed through their insurance). “They’re supposed to self-quarantine, take time off from work, but the correctional officers are so understaffed,” says Jenkins. “They’re disregarding the rules because they think their presence is needed.”
An anonymous officer at Arizona State Prison Complex-Yuma says that supervisors were not informing staff if inmates were infected, and that they were being forced to work in units with known cases. Another Yuma officer told Jenkins that everyone in the facility was trying to survive: “You know, right now I don’t think it’s inmate versus staff,” he said. “Right now, we are all trying to come together and get through this.”
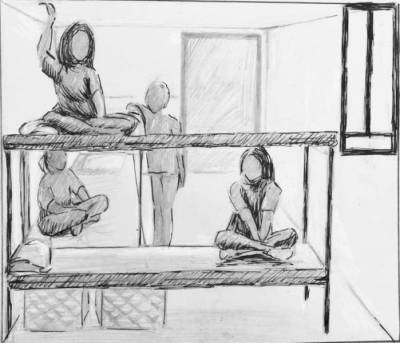
At Indiana Women’s Prison, inmates are stuck in sweatbox cells for up to 20 hours a day to help reduce spread, Jake Harper reports for WFYI. Two to four people are housed in the units, known as “cottages,” which have no air conditioning, toilets, or sinks. “You’ve got these inmates sitting inside sweating, unable to move,” Harper told Science Friday over the phone. “It might be preventing the spread of disease, but it has other consequences.”
The coronavirus lockdown has caused some to become dehydrated because they choose not to drink water out of fear of having an accident, while others are taking less of their medication known to cause frequent urination. Inmates also have limited supplies of feminine hygiene products, causing them to need the bathroom more often during menstruation.
Avenal State Prison in California’s Central Valley reported the second largest coronavirus outbreak among the state’s correctional facilities. The prison has reported 1,298 cumulative cases among both the incarcerated population and staff, as of July 30. But, before COVID-19, the prison had seen spikes of another disease: valley fever.
Unlike COVID-19, valley fever is not transmitted from person to person. The disease is caused by inhaling a fungus commonly found in soil and dust in the American Southwest, which triggers flu-like symptoms in patients, but can be chronic and even deadly. More than 800 men incarcerated at Avenal contracted valley fever, Kerry Klein reports at KVPR Valley Public Radio. Hear stories from the former inmates about living life after prison, with valley fever.
Paige Pfleger is a reporter for WOSU in Columbus, Ohio. She’s especially interested in the intersection of public health and criminal justice.
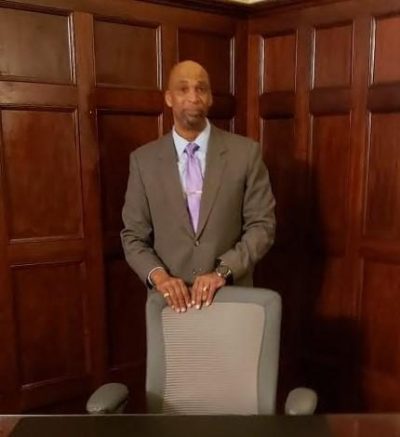
Jimmy Jenkins is a senior field correspondent at KJZZ in Phoenix, Arizona and a contributor to NPR’s Election 2020 and Criminal Justice station collaborations.
Zinzi Bailey is a social epidemiologist at the University of Miami in Miami, Florida.
Lauren J. Young was Science Friday’s digital producer. When she’s not shelving books as a library assistant, she’s adding to her impressive Pez dispenser collection.
Kathleen Davis is a producer and fill-in host at Science Friday, which means she spends her weeks researching, writing, editing, and sometimes talking into a microphone. She’s always eager to talk about freshwater lakes and Coney Island diners.
John Dankosky works with the radio team to create our weekly show, and is helping to build our State of Science Reporting Network. He’s also been a long-time guest host on Science Friday. He and his wife have three cats, thousands of bees, and a yoga studio in the sleepy Northwest hills of Connecticut.