Happy (Holiday) Testing Season!
17:01 minutes
This story is a part of Science Friday’s coverage on the novel coronavirus, the agent of the disease COVID-19. Listen to experts discuss the spread, outbreak response, and treatment.
The holiday season has snuck up once again, leaving many people to figure out familiar logistics: If travel will be involved, who to see, and what will be for dinner. But of course, we’re still in a pandemic, so questions of safety remain. At the end of the day, we want to keep our families, friends, and loved ones healthy.
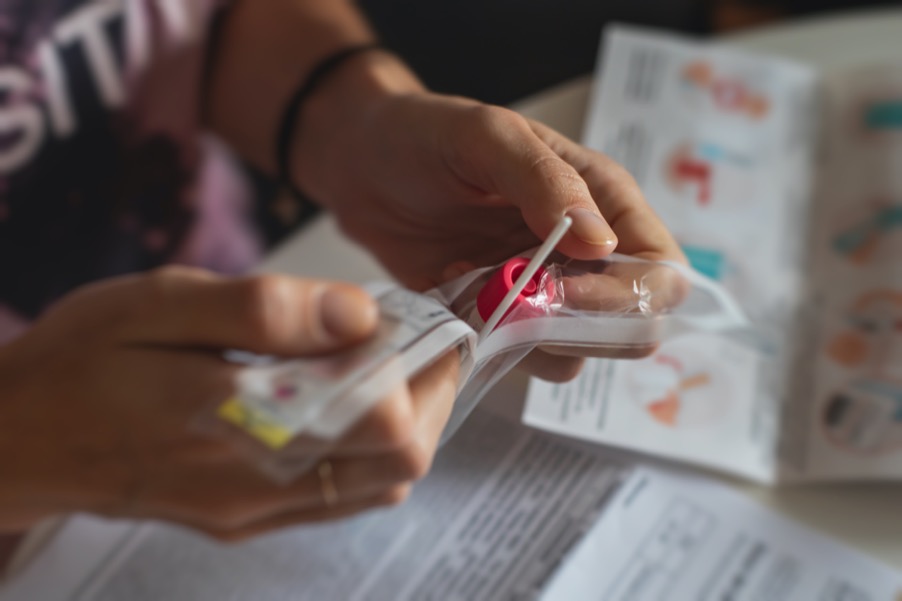
COVID-19 tests are becoming a popular tool, helping many people make social situations safer. Quickly swabbing your nose or spitting in a tube can indicate if someone has been infected with the coronavirus. But with so many options available, and a big season of holiday get-togethers up ahead, many are wondering what kind of test is best—and when is the best time to get tested?
Joining guest host Roxanne Khamsi to talk through COVID-19 testing questions are Dr. Céline Gounder, epidemiologist and professor at New York University’s Grossman School of Medicine in New York, and Dr. Alex Greninger, assistant director at the clinical virology laboratories at the University of Washington Medical Center in Seattle.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Céline Gounder is Editor-at-Large for Public Health at KFF Health News in New York.
Alex Greninger is Assistant Director of the Clinical Virology Laboratories at the University of Washington Medical Center in Seattle, Washington.
ROXANNE KHAMSI: This is Science Friday. I’m Roxanne Khamsi. Like a lot of people, I feel this holiday season really has snuck up on me. And like most holiday seasons, I’ve got logistics to figure out. It’s tricky because there’s a chance I might be flying internationally to see family. But of course, we’re still in a pandemic, so questions of safety remain, and at the end of the day, all of us want to keep our families, friends, and loved ones healthy. How do we do it?
COVID-19 tests are proving to be a popular tool for a lot of people to figure out whether a social situation is safe. Quickly swabbing the nose or spitting in a tube can tell you if you have COVID. But with so many options and a big season of holiday get-togethers ahead of us, a lot of people are wondering, what kind of test is best and when?
The whole thing can become overwhelming pretty quickly. Joining me now to answer these questions are my guests Dr. Celine Gounder, epidemiologist and Professor at New York University’s Grossman School of Medicine in New York City. Hi, Celine.
DR. CELINE GOUNDER: Hey.
ROXANNE KHAMSI: And Dr. Alex Greninger, Assistant Director of the Clinical Virology Laboratories at the University of Washington Medical Center in Seattle. Hi, Alex.
DR ALEX GRENINGER: Hi. How’s it going?
ROXANNE KHAMSI: Alex, last year we were having a lot of the same conversations about how to have get togethers safely. But a lot of things have changed since then, right? Can you walk us through what are the big differences between last year’s holiday season and this one?
DR ALEX GRENINGER: Well, I think the major difference between last year’s holiday season and this year’s holiday season is the vaccines. We have the vaccines this year. That’s really probably the most important thing that changed. We also have some new testing modalities, so rapid tests were approved at the time, but many of them were not really available over the counter or could be bought easily by people. That’s a new option. We still have to use all of the different modalities we have to prevent transmission with masking, ventilation, and the whole pandemic playbook here is really important.
ROXANNE KHAMSI: Yeah, I think those things are definitely big changes, and yet, as you mentioned, some of the stuff that we tried to do last year remains. Celine, how about you? Do you feel safe enough to get together with loved ones for the holidays?
DR. CELINE GOUNDER: Well, I think there are a couple of questions I ask myself. I think a good framework for people who are planning their holidays, I would say, number one, think about who’s going to be there. Is anyone who’s really vulnerable– so when I mean really vulnerable, I’m talking about the elderly, people with immunocompromised conditions, maybe it’s an elderly grandparent who lives in a nursing home. These are the people who are most likely to have a severe complication from COVID, even if they’re vaccinated. They are at higher risk for breakthrough infection that can progress on to severe COVID.
I really think you should be conscious of who’s going to be there. Other people may have similar but different issues where it’s really too high-risk for them to get an infection over the holidays.
ROXANNE KHAMSI: Are you taking any special steps yourself to ensure that you and your family will be safe?
DR. CELINE GOUNDER: Well, all of us, with the exception of my two-year-old niece, will be vaccinated. My six-year-old niece just got her first dose of the Pfizer vaccine. She’ll get her second dose before the holidays. My mom, who is elderly, has recently gotten her third dose of the Moderna vaccine. We’ll all be– with the exception of my two-year-old niece, we will all be fully vaccinated before Christmas. As Alex said, you have to think about this as the full pandemic playbook– of layering different things because none of them is perfectly 100% protective.
In addition to getting vaccinated, I do think rapid tests are probably the easiest thing to implement without disrupting your holiday activities.
ROXANNE KHAMSI: Mm-hmm. Yeah, we’re so we’re going to be layering. Just like we layer our winter clothes, it’s all about layering these different protective measures and then maybe throwing in some rapid tests, too, for good measure.
DR. CELINE GOUNDER: Yeah, I think that’s right. I love your metaphor of the winter layers. I think that’s right. You know you have one layer that blocks out the rain. You have another that’s warmer. I think that’s a similar kind of thing here.
ROXANNE KHAMSI: So, Alex. Let’s talk about testing. You run a massive testing laboratory in Seattle how many COVID-19 tests has your lab in processing?
DR ALEX GRENINGER: Yeah, so since the beginning of the pandemic, we’ve done about 3.6 million tests. We were one of the first labs to go live– clinical labs in the country. For us, that’s about 72 years of testing in the last 20 months. That would be across all analytes, but that’s just for COVID. It’s really an incredible amount of testing that we’ve done.
Those are the ones we know– which is great. We get to do PCR testing. We can get high-sensitivity. Those data get reported directly to public health, which is fantastic. The new thing is, basically the development of these rapid tests be able to provide that in the household, or at the workplace, or many different other locations.
I wish those tests were getting reported to public health as well, but they are, like we said, the different layers that can be used to prevent transmission and help people understand what their status is and how to interact with the health care environment, as well.
ROXANNE KHAMSI: Just to note, you’re in an airport, also, as you’re talking with us. You’re probably thinking about the testing in action as people are traveling. You’re kind of getting a preview of the holiday season to come.
DR ALEX GRENINGER: Yeah, definitely. I mean, if you’ve been to an airport recently, I mean, it’s almost back to 2019. Maybe like 20% lower. It’s a little bit lower, but it’s still it’s pretty hopping. There’s a different attitude towards the virus. I think a lot of people expect, over the holidays, we’re going to see a much higher rate of transmission. A lot more cases around the country, unfortunately.
ROXANNE KHAMSI: One of the things that we’re talking about here is the different test options we have. Alex, you were saying that you’ve been running millions and millions of tests, which is phenomenal, but there’s PCR, there’s antibody tests, some of these can take a few days to process, and others are pretty instant. Would you recommend to listeners to have one type of testing over another for the holiday season?
DR ALEX GRENINGER: I mean, there’s a lot to say for rapid tests because they give you that result at that moment, right? I mean, they’re are hundreds times less sensitive from an analyte standpoint, but the part that they’re missing is maybe a little less important overall. From terms of where they’re missing those infections, are people who have lower viral loads, potentially a little less infectious. There’s a lot to say for different testing modalities, but I do like rapid testing from the standpoint of get the result right then, and you know that status.
If you’re about to go to a dinner party, or you’re about to interact with people, you know the situation right then. With PCR testing, the advantages are it’s usually collected and observed by someone else. It’s run by someone else. You can use that results for many different purposes, whether it’s travel or meet some of the OSHA requirements for workplace-required testing– that is helpful. As well as it gets reported to public health. I think that’s really important that our policymakers have a good understanding of how many tests are being done, how many infections are being picked up. Really, that’s one of the most important things is the policy response that we have for the virus. They’re both helpful, but I do think, from some of these holiday standpoints, it actually is– rapid testing has a lot to offer as well.
DR. CELINE GOUNDER: Roxanne, if I could add to that, just briefly, I think the power of rapid testing is that it’s rapid, but also that it’s picking up the people who are really infectious or contagious to others. If the purpose here is really to reduce transmission, rapid tests are a really powerful tool. It may not be what we want to use in the hospital when somebody is sick, and we’re trying to figure out what you have, but that’s not really the purpose here. It’s really just to figure out are you contagious to other people? For that purpose, the rapid tests are really great tools.
ROXANNE KHAMSI: That’s a lovely way to look at the advantage of rapid tests. I’m curious because, in the past months of the pandemic, I have heard concerns that at-home testing isn’t always as accurate. Alex, I’m wondering, do you have any thoughts on whether at-home testing is as accurate as what happens in the lab?
DR ALEX GRENINGER: I mean, they’re accurate enough. They are, like I said, from an analyte standpoint, they are less sensitive, but as Dr. Gounder said, they are also picking up the people who are most likely to be infectious. I think what’s most important to highlight when it comes to testing or any of this is the layers we talked about before, as well as what you do with the information and how you act.
I mean, I’m going to use the University of Washington Football Team from last year that basically did not get to go to the Pac-12 championship game because they had an outbreak in the football team. They were getting daily antigen testing and weekly PCR testing, and yet the risk that they themselves were at, whether from their household transmission or from the team itself and the close quarters, there are still 23 other hours during the day where you’re not getting that result. While it’s very helpful, you’ve got to, as well, sort of de-risk yourself and think about the other layers that you’re bringing in if you want to avoid getting infection or having transmission.
ROXANNE KHAMSI: I mean, this is a lot to think about. As we’re talking, I’m also recalling that I was in an airport not that long ago. I tried to get access to a rapid test for travel and ordered one online, but by the time it had arrived, I was already on my flight, so I had to find other testing options. I’ve heard that for a lot of people, finding rapid tests can be kind of a mixed bag. In some places, they’re pretty accessible, and then other places that are kind of impossible to find. Celine, do you have any thoughts on why supplies have fluctuated so much? I know you’re not running the supply chains, but I’m curious if you have observed this kind of phenomenon.
DR. CELINE GOUNDER: Yeah, I’ve certainly seen it firsthand, and there are a number of different bottlenecks. One, you have the FDA and their regulatory framework. They’re not really set up to approve tests for a public health purpose, as opposed to a diagnostic purpose. When you’re talking about testing to assess if somebody’s contagious– not to make a diagnosis of COVID for their medical care– the purpose we’re talking about here is really a public health purpose. The FDA is not really set up to do that.
In addition, they just weren’t set up to approve this many new rapid diagnostic tests in the context of the pandemic. There have been some moves recently from the White House to facilitate more rapid approval in the future. The NIH has recently announced a new program where they will, in fact, do a lot of the testing for the test kit developers so that there’s a much more standardized, streamlined process leading up to an FDA approval. In addition to some of these regulatory issues, there have been, as you alluded to, there have been issues with the supply chain. The different components that go into making a test, unlike in other countries, like the UK, for example, where there was investment by the government pre-purchasing tests so that manufacturers knew there was going to be a certain demand. Knowing that you have a predictable demand makes it a lot easier to ramp up supply.
I think there has been really bad messaging around how to use rapid tests. What’s the purpose of rapid tests? I think everyone had really doubled down on vaccinations. As we talked about earlier, vaccinations are really important. They might be our most powerful tool in the toolbox, but at least for the foreseeable future, we’re going to need to layer other tools, other approaches.
Then finally, I think what you alluded to at the beginning, which is it’s really hard to find a test, and they’re really expensive. You’re still talking about, easily, $25 a test in many places. For listeners, a couple places where you might look to for a lower-priced test would include IHealth labs I health L A B S .com. They currently are available at $7 a test. There are a couple different retailers, Walmart, Amazon, and Kroger, who have agreed to sell their test at cost for $14 over the next three months. Many others, CVS, Walgreens, and the like, are also selling these rapid tests. It’s just a question of can you get your hands on them.
ROXANNE KHAMSI: As you’re saying these prices, I’m thinking maybe I’ll make them stocking stuffers. Alex, can you say a little bit about what’s the ideal time to do a COVID test ahead of, let’s say, Thanksgiving, which is coming up on Thursday.
DR ALEX GRENINGER: Right, so whatever test you’re getting, the most important thing is that you’re able to get that result and then act on it– whether it’s antigen testing or PCR testing. If it’s PCR testing, you do have to factor in the turnaround time at the lab, which can be different in different locations. Generally, you probably want to get tested probably on Tuesday, maybe Wednesday morning, depending on different locations. That’s one of the problems, right? That there’s still that time that can pass, and you can still have the virus.
For rapid testing, 15 minutes, you want to do it right before you go to dinner while you’re headed over to someone’s place or whatnot because you can get that result. You can know immediately what your status is at that moment. That’s really just want to make sure that you get the result with time and the ability to act on it. Otherwise, it’s just you’re just getting tested.
Shelf life of them is quite long. Right? They’ll be available. You can get some now for Thanksgiving, even get it for Christmas. They’ll be stable during that entire time period. You’ll be OK. It’s not too late.
ROXANNE KHAMSI: The worst thing would be to have like dessert, and then get your result and find out that you’re positive.
DR ALEX GRENINGER: Right, exactly.
ROXANNE KHAMSI: OK, great. Well, thanks for clarifying that. Just to pause here, I’m Roxanne Khamsi, and this is Science Friday from WNYC Studios. We’re talking about COVID testing ahead of the holidays with Dr. Celine Gounder and Dr. Alex Greninger. Celine, I know you have very strong thoughts about boosters. News came out today from the FDA. They’ve authorized COVID booster shots for all adults in the US. The CDC still needs to sign off on it, but it’s a really big step. That’s after several states have already recommended that residents get the booster. Celine, would you recommend that people get boosted now.
DR. CELINE GOUNDER: The people who should absolutely get boosted now are the elderly. There’s different ways of defining the elderly depending on the study, but definitely, if you are 65 and older, you should absolutely get a booster now. We know that that group, the elderly, has something we call immunosinesis which is basically aging of the immune system where your immune system does not respond as well, up-front, to vaccination. Giving you an extra dose of the vaccine will help you generate a more robust, durable response to vaccination.
The other groups that really would benefit from an extra dose of vaccine now are people who are highly immunocompromised– for example, somebody who’s had a solid organ transplant. Then people who live in nursing homes. This is really the setting, in particular, where we have seen people who have infections after vaccination, and those infections can turn bad. In other words, those people go on to severe disease, hospitalization, and death, unfortunately not infrequently. It’s really important for people who are living in a nursing home, who work in a nursing home, if you’re planning to travel to visit somebody in a nursing home to also be more cautious. The residents and staff of nursing homes and other long-term care facilities should absolutely receive another dose of vaccine now.
ROXANNE KHAMSI: People in regular Thanksgiving settings where there’s a mix of different generations, if people want to get boosted who might not be falling into those categories that you mentioned, if they want to get boosted to get the most protection for Thanksgiving, is it too late?
DR. CELINE GOUNDER: If you’re wanting to do that, I think you probably want to do that about two weeks prior to the holiday. I think you have to be very clear about what it is you’re achieving. I do think there’s a danger that some people think that getting a booster means that, now, you don’t have to worry about COVID anymore. You’re Superman. You’re not ever going to have to take other precautions, and that is the danger here.
By giving you an extra dose of vaccine, we know that will boost your antibody levels over the short term. We do not know what the impact will be on your underlying immune memory, which is really what you’ll revert back to, fall back to within six months or so. I would just be very cautious about interpreting what that action means for you and for others.
ROXANNE KHAMSI: A booster is not a free pass, and we should definitely continue to layer as we get through the holidays.
DR. CELINE GOUNDER: That’s right. That’s right. Continue to layer.
ROXANNE KHAMSI: We’ve run out of time. I’d like to thank my guests Dr. Celine Gounder epidemiologist and Professor at New York University’s Grossman School of Medicine in New York City, and Dr. Alex Greninger, Assistant Director of the Clinical Virology Laboratories at the University of Washington Medical Center in Seattle.
DR. CELINE GOUNDER: Of course, by everyone. Bye, everyone.
DR ALEX GRENINGER: All right Thanks a lot. I appreciate you all. Cheers.
Copyright © 2021 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Kathleen Davis is a producer and fill-in host at Science Friday, which means she spends her weeks researching, writing, editing, and sometimes talking into a microphone. She’s always eager to talk about freshwater lakes and Coney Island diners.