Looking To The Genome To Track And Treat The New Coronavirus
17:18 minutes
This story is part of Science Friday’s coverage on the novel coronavirus, the agent of the disease COVID-19. Listen to experts discuss the spread, outbreak response, and treatment.
As of Thursday, March 5, Washington state has reported over 30 cases of COVID-19, the disease caused by the coronavirus, SARS-CoV-2. To better understand the pathogen and the disease, scientists have sequenced the genome of the virus from two of the patients. Kristian Andersen, an immunologist at Scripps Research who uses genomics to track the spread of diseases, discusses how the genetic information from these patients can help determine the spread of the virus globally. Plus, Ralph Baric, a coronavirus researcher at the University of North Carolina at Chapel Hill, talks about developing vaccine and drug candidates for COVID-19 and how the genomic sequences from this outbreak can be used to help create treatments.
Invest in quality science journalism by making a donation to Science Friday.
Kristian Andersen is an associate professor of Immunology and Microbiology at the Scripps Research Institute in La Jolla, California.
Ralph Baric is a professor of Microbiology and Immunology at the University of North Carolina Chapel Hill in Chapel Hill, North Carolina.
IRA FLATOW: This is Science Friday. I’m Ira Flatow. Currently, there are a little over 200 confirmed cases of the coronavirus in the US affecting 18 states with New Jersey and Tennessee to be the latest to report cases. Washington State alone has 70 confirmed cases.
Scientists were able to sequence the genomes of two of those patients in that state. And even since the beginning of the outbreak in China, researchers have been quickly putting together genomic data and sharing it with one another. We’re going to talk about what we know about the genome of the virus, how it can be used to track spread, and how that information might be helpful when developing drug and vaccine treatments.
If you have questions, we’d like to hear from you. 844-724-8255. You can also tweet us @SciFri. Let me introduce my guest. Kristian Andersen is an Associate Professor of Immunology and Microbiology at Scripps Research in La Jolla, California. Welcome back.
KRISTIAN ANDERSEN: Hi, Ira. Thanks for having me back.
IRA FLATOW: You’re welcome. Ralph Baric is a virologist who has studied coronaviruses for 30 years. He’s a Professor of Microbiology and Immunology at the University of North Carolina at Chapel Hill. Welcome to Science Friday.
RALPH BARIC: Hello, Ira. Pleasure to talk with you.
IRA FLATOW: Thank you. Kristian, Washington State, as I say, has 70 confirmed cases of COVID-19 as we mentioned. Scientists sequenced the genomes of the viruses from two of those patients. Well, what does the data tell us about how the virus is spreading in that community?
KRISTIAN ANDERSEN: Yeah. So this is a very interesting study from the Seattle Flu Study led by Trevor Bedford at the Hutch. And what they did here was that they had a travel-associated case back in January of this year and that was sequenced by the CDC. And then later on in February, the Flu Study started looking at flu suspected cases to see if they could find any COVID-19 cases in that. And they came up with a single positive case that they then sequenced.
And then once they sequenced that, they realized that this linked back to this very first case that they had sequenced in January. So what that data really strongly shows is that the virus has been circulating in the Seattle area for at least six weeks. We have just been missing cases all up until now.
IRA FLATOW: And how can we stop missing cases?
KRISTIAN ANDERSEN: Yeah, so one of the main issues in the United States here is that we have really been woefully unprepared to take this virus on. Our testing capacity has been much, much too low. And so the test case, we’re saying, how could you get tested with this up until recently included travel to China.
But of course, the problem is that we have many COVID-19 cases all across the world. And all the tests until very recently also had to be done by the CDC. So our ability to test for cases has been very, very, very lacking all the way down to similar to what we have seen in Iran. So for a while we have simply just been missing cases because we haven’t been able to look for them.
IRA FLATOW: So we really don’t have a good idea even outside of Seattle how this spread has happened?
KRISTIAN ANDERSEN: No. I think one of the main concerns that we see is that we have seen early on in the outbreak of detecting cases here that we have a lot of fatalities. And when we start seeing fatalities it really means that you have significantly more spread in the community than you are currently realizing.
So the estimates in the Seattle area is probably maybe 1,000 to a couple of thousand by now. But of course, what we have to remember is that this virus tend to– like the outbreak tends to double about every week or so. So we’re going to see it long– a stark increase in the number of cases as we are now starting to look for them.
IRA FLATOW: And would it be– would it be helpful to test everybody because we keep hearing that the virus may be asymptomatic, right?
KRISTIAN ANDERSEN: Yeah, so I think– yeah, so currently that’s definitely not possible because it’s– that would require way more testing capacity than we do have. But I think anybody with a fever or flu-like symptoms at this stage should be tested, of course, for flu and other infectious diseases, but if possible, also for COVID-19.
IRA FLATOW: Ralph, let’s talk about this coronavirus. As I said, you’ve been studying it for 30 years. What makes this virus different from any other coronaviruses?
RALPH BARIC: Well, of course, the model coronavirus was SARS coronavirus, which emerged in 2003. It caused about 8,000 cases and had a 10% mortality rate. The major difference between the ancestral SARS coronavirus strain and SARS-2, which emerged in 2019, was that most of the SARS coronavirus 2003 strain infections were extremely serious. Anyone who became exposed became very ill. And then they didn’t really transmit until they had serious disease. And so the outbreak was very vulnerable to contact tracing and quarantine.
In this case, this virus can have asymptomatic infections, very mild infections. It can transmit prior to development of severe disease. And so it has many more flu-like characteristics. And this makes it much more transmissible in the community setting and much more difficult to control.
IRA FLATOW: And the fact that I understand or I’ve heard that the incubation period is what, two weeks?
RALPH BARIC: It’s two to 14 days with an average of around five to seven days.
IRA FLATOW: Does that make it hard to track or also diagnose?
RALPH BARIC: Well, the initial CDC screen was at five major airport portals of entry based on temperature. With a four or five-day incubation period where you’re infected without fever, then those people would slip through the screening. Then the fact that you had asymptomatics that may not develop fever, or low-grade fevers which would be subject to fever reducers, they would slip through the system as well.
So the system that was set up was porous. It was unfortunate, I think, that they didn’t set up secondary screening at major hospitals that look for transmission networks that had been– became established early in the outbreak.
IRA FLATOW: If I go to my doctor or if I go to the emergency room and they suspect that I may have it, can they just phone up a test kit? Kristian, Ralph?
RALPH BARIC: Well, right now I think 700 people have been tested in the United States. The main problem was that the initial test that was rolled out by the CDC had a performance issue and gave false positives, so they had to start over. This led to a huge backlog. And then it was further complicated in that the case definition required some linkage to travel from China. And as the virus began to appear in other regions of the world, that obviously allowed people to slip through the network.
So we don’t have enough cases. I think the projections are we would have about 75,000 cases of– kits available to screen people in the US at the end of this week. In contrast, a place like South Korea is screening 10,000 cases or 10,000 patients a day.
IRA FLATOW: Why can’t we get their kits?
RALPH BARIC: That’s a good question.
IRA FLATOW: If they got so many kits, why can’t we just import them? Pay them for it.
[LAUGHTER]
It was a serious question. If they know how to–
KRISTIAN ANDERSEN: Well, yeah–
IRA FLATOW: If they know how to do it, why don’t we just take their stuff?
RALPH BARIC: Well, the WHO–
KRISTIAN ANDERSEN: Yeah.
RALPH BARIC: –also has tests. New York City then has recently developed and certified its own test. I think it’s a– it was a fundamental error in pandemic preparedness.
IRA FLATOW: Kristian, you agree?
KRISTIAN ANDERSEN: Yeah. I absolutely agree with this. The fact is that the WHO and China as well have had very functional tests for months now, while the US was trying to develop its own test, which unfortunately turned out to be faulty in the beginning. And then the rollout has also been problematic.
So for two– the first two months of the epidemic where we really should have done everything we could to prepare, it was used trying to develop, test, and roll them out, that then turned out not working. It’s very unfortunate because this is really the most critical first step when it comes to preparedness.
IRA FLATOW: Mhm.
RALPH BARIC: I agree completely.
IRA FLATOW: Let’s talk about the following it– the disease around the world. Kristian, let me ask you. I know that Italy is reporting quite a few cases, right? Do we have any genomic information or any idea of how the virus– that Italian virus is spreading globally?
KRISTIAN ANDERSEN: Yeah, so we have a little bit of– so yeah, as you’re saying, Italy have about 4,000 cases now– described cases. It’s really important to make this distinction between what is described and the true number of cases, because that’s going to be much different in places like Italy and certainly also in a place like the United States. Italy themselves unfortunately haven’t produced a lot of sequencing data, but we’re starting to see travelers from Italy traveling to places like Brazil, Mexico, Finland, Germany, and other places.
And it gives us a sense of what’s actually going on in Italy. And some of the things that we can see is that Italy has multiple clusters of transmission chains. So there are multiple introductions into Italy itself and then these introductions launched their own chains that we’re now seeing circulating in Italy. And then, of course, because there’s so many infections and people traveling to Italy, we’re now seeing these exportations out of Italy to other countries as well.
IRA FLATOW: Ralph, you’ve been working, as I said before, on coronaviruses and treatments for decades. Where do we stand with treatments? I remember back in 2009– I just started throwing out old boxes of Tamiflu this week for the H1N1 virus that was– that was a pandemic. Do we have any treatments in the works for not just precautionary like a vaccine, but something that will work?
RALPH BARIC: So there’s been several drugs that have been in clinical trials both for SARS, the closely related Middle East respiratory coronavirus that emerged in 2012, and there’s even been clinical trials going on with the SARS-2 viruses in China. One drug that’s been tested quite a bit is HIV protease inhibitors, lopinavir and ritonavir. Their efficacy is mixed and still debatable within the field.
Our own group worked carefully and closely with Gilead over the past five years as part of a Center for Excellence in Translational Research that’s run out of University of Alabama with a fellow named Rich Whitley. And we had screened a large number of drugs from Gilead and identified a drug called remdesivir, which is very effective against SARS and MERS, and also the new SARS-2 strain, as well as a large panel of related SARS and MERS-like viruses from bats, as well as– and for contemporary human coronavirus strains. So that drug is currently in trials in two different cohorts in China. And there’s a clinical trial study with cases and controls here in the United States as well.
IRA FLATOW: Will they speed up that trial at all?
RALPH BARIC: Well, the limit– the bottleneck is always the availability of cases that can be enrolled. The mathematical modelers argue that there should be fair numbers of cases available over the next two weeks.
IRA FLATOW: No shortage of cases is what you’re saying.
RALPH BARIC: I think that’s true.
IRA FLATOW: Anthony Fauci from the National Institute of Allergy and Infectious Diseases put the timeline for a vaccine at one to one and a half years, Ralph. How does the process work when there’s a current outbreak of disease? What– is that– that sounds like– and he said this many, many times. He’s been contradicted by the White House. How does– how does that work?
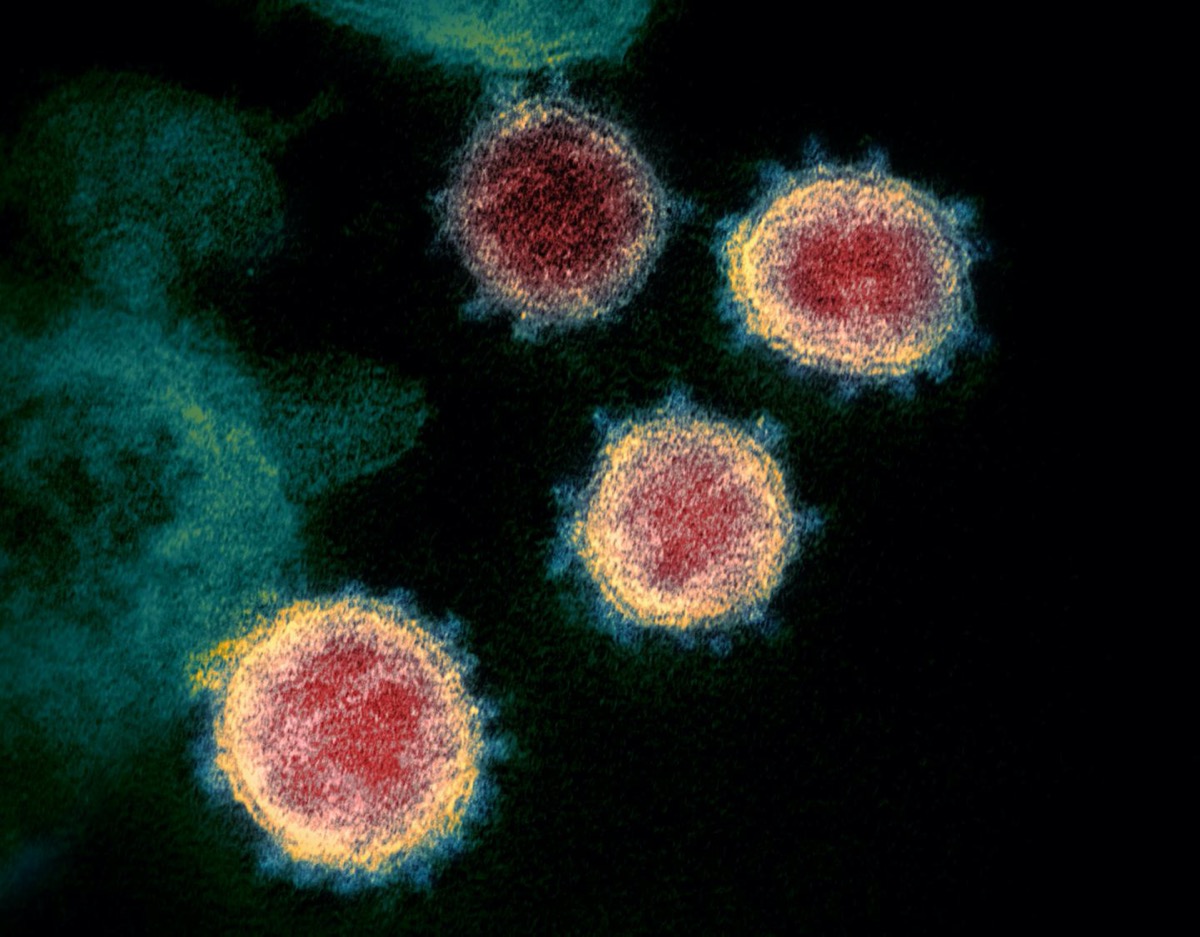
RALPH BARIC: So the process begins when either the sequence or the virus becomes available. So when the Chinese first published the sequence of the new virus on January 9, 2020, many labs and many companies, including my own, synthesized the spike glycoprotein, which is the major surface glycoprotein that gives the virus its unique appearance in the electron microscope. And then they place that in expression vectors or synthesize it as a recombinant protein. And then they, within about two to three weeks, have candidate vaccines that are ready to go.
So the next phase is then to demonstrate that the– that you can produce sufficient quantities of that material that is in the right confirmation. So in other words, the neutralizing epitopes that are going to be– and the T-cell epitopes that are going to be critical for protective immunity need to be properly presented in the context of the host. And so that means in vitro work has to be done.
And then you have to go into animal models to assess is it immunogenic? Does it make a protective immune response? Which is typically associated with neutralizing antibodies for coronaviruses. And then those animals need to be challenged with a virus in a lethal challenge model that recapitulates many of the disease features of the virus.
IRA FLATOW: I hear you saying it’s a long process. [LAUGHS]
RALPH BARIC: Yeah, it takes– it takes about a year. And then you have to move into phase one trials in humans and phase two trials. And there are complications in SARS coronavirus vaccine design which could delay the process further.
IRA FLATOW: I’m Ira Flatow. This is Science Friday from WNYC Studios talking about the coronavirus. Let me see if I can get one call in before we run out of time. There’s so little time. Let’s go to Rebecca in Cambridge, Mass. Hi, Rebecca.
REBECCA: Hi, how are you?
IRA FLATOW: Hi, there. Thank you. Go ahead.
REBECCA: Thanks for taking my call. I had a question about these cases that have broken out in this country and across the world. How come we’re not hearing of any school-age children or younger children getting the illness? Are there any thoughts or reasoning behind that that we know of?
IRA FLATOW: Good question. Kristian, Ralph?
KRISTIAN ANDERSEN: Yeah, so I think this is a really peculiar thing. There’s now been studies showing that they actually do get the virus. They just don’t seem to get the disease. What exactly is going on there is unclear. But coronaviruses, in general, we are exposed to a lot as children– the cold– common cold-type of viruses. So whether there could be any potential cross-protection there for those sort of exposures is an open question. But I think it’s very, very interesting that we really don’t seem to see the disease. But the infection does occur in children.
IRA FLATOW: I have a quick tweet from Lisa in Sacramento who asks, “Do UV sanitizing wands affect the DNA? Could they help disinfect surfaces instead of the alcohol that we’re telling people?”
RALPH BARIC: You said UV?
IRA FLATOW: Yes, ultraviolet.
RALPH BARIC: Ultraviolet. Yes. Ultraviolet will neutralize virus infectivity. We use it to sterilize hoods sometimes in the BSL-3 facility.
IRA FLATOW: Mm-hmm. So where do you see this happening or ending up? Or is this just going to be a slow drip, drip of cases, Ralph, that you see happening more and more in the US?
RALPH BARIC: Well, I think the model globally is that there will be a slow increase of cases followed by almost explosive increases in cases like has occurred in Italy, and South Korea, and in Iran. And I guess the question is, is the US at the apex of that massive increase of cases or not? Most of the epidemiologists who do mathematical modeling and disease prediction about how case rates are going to increase argue that we may be facing some very, very difficult times ahead.
IRA FLATOW: Because we’re talking a geometric progression here, right?
RALPH BARIC: That’s correct.
IRA FLATOW: Kristian, do you agree?
KRISTIAN ANDERSEN: Yeah, I agree. I think we’ll probably see an exponential increase in cases in the United States here over the next few weeks at least. And I think, again, the really, really critical thing here is that we need to ramp up that diagnostic testing capacity. All states need to be able to do this. Hospitals need to be able to do this. And right now this is just not in place. So I really think a lot of focus need to be put there, so we can try and understand how big of a– big of a problem are we actually dealing with here.
IRA FLATOW: Thank you, gentlemen. Kristian Andersen from Scripps in La Jolla. Ralph Baric at the University of North Carolina in Chapel Hill. Thank you both for some great talking to us about it.
Copyright © 2020 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Alexa Lim was a senior producer for Science Friday. Her favorite stories involve space, sound, and strange animal discoveries.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.