Fauci Says Majority Of U.S. Adults Likely To Be Vaccinated By Late Summer
26:02 minutes
This story is part of Science Friday’s coverage on the novel coronavirus, the agent of the disease COVID-19. Listen to experts discuss the spread, outbreak response, and treatment.
We’re about a month shy of a big anniversary: one year since the World Health Organization officially labeled COVID-19 a pandemic. Since then, a lot has changed—and a lot has not.
We have more information than ever about COVID-19, but there are still a lot of unknowns about the illness. While about 40 million people in the U.S. have received at least one dose of a vaccine, it’s unclear when we can expect to return to a sense of normalcy.
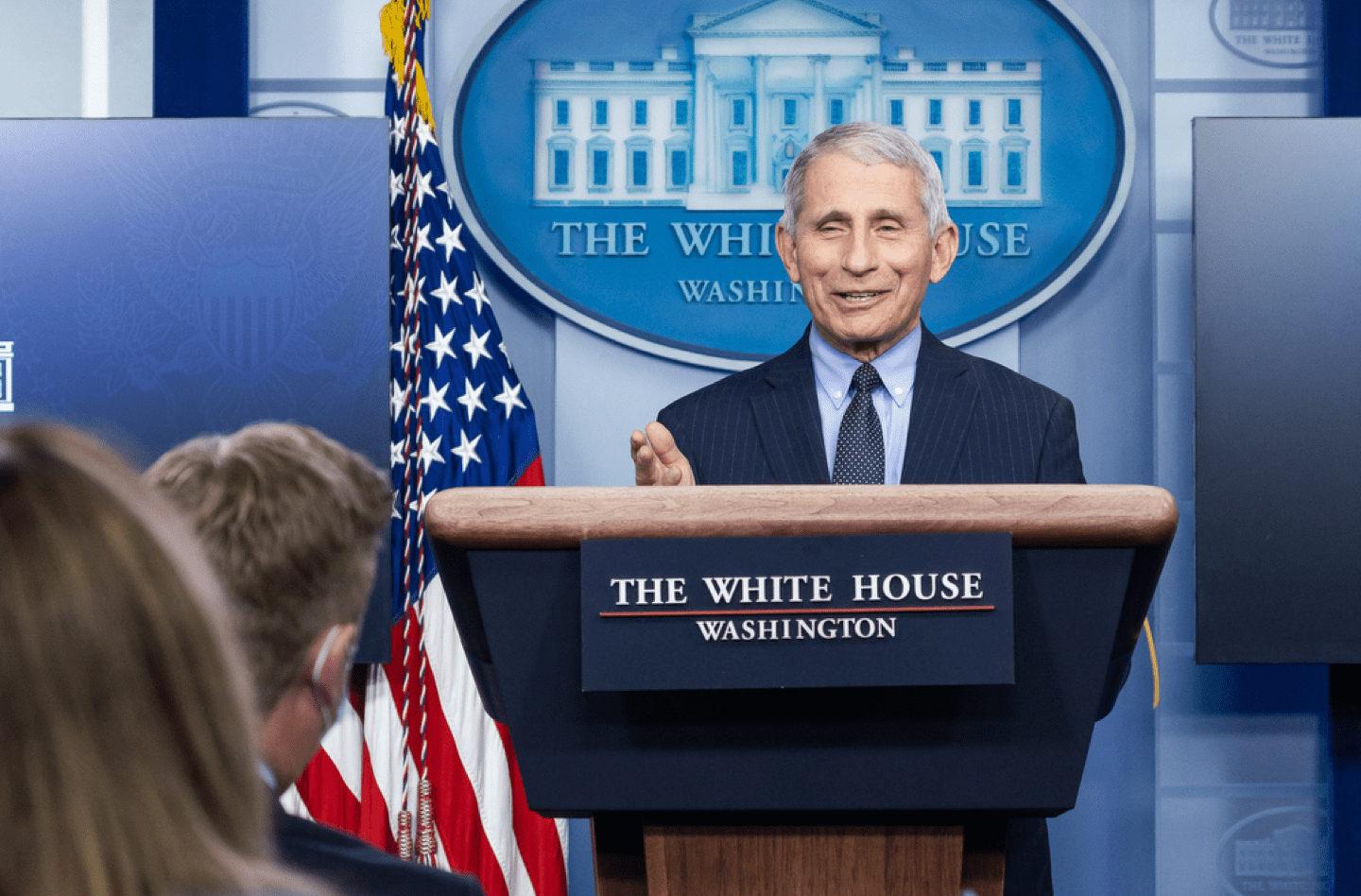
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, joins Ira to shed some light on the latest news about variants and vaccines—and the light at the end of the COVID-19 tunnel.
He predicts vaccines are likely to be open to all adults starting in May or June. “By the time you get everyone vaccinated who could be vaccinated, that’s going to take several months,” Fauci says. “So it won’t be until the end of the summer.”
Fauci and Ira also discuss when it’s ok for families to get together without a laundry list of precautions, as well as his legacy from decades at the NIH.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Anthony Fauci is the former Director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health, and author of On Call: A Doctor’s Journey in Public Service. He’s based in Washington, DC.
IRA FLATOW: This is Science Friday. I’m Ira Flatow. We’re about a month shy of a big anniversary, the one year anniversary of the World Health Organization labeling COVID-19 a pandemic. It was a nerve wracking time. A lot has changed and a lot has not. The good news– we have more information than ever about COVID-19 and vaccinations are happening all over the world. But there are still a lot of unknowns about the illness and when we can get back to normal.
One thing that has stayed the same– Dr. Anthony Fauci is still a trusted source of COVID-19 information. And he’s also my guest this week. Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases in Bethesda, Maryland and a recipient of the Presidential Medal of Freedom. Nice to have you back. Thank you for joining us this hour.
ANTHONY FAUCI: My pleasure, Ira.
IRA FLATOW: Couple of weeks ago, I interviewed Dr. Benhur Lee of Mount Sinai about the virus. And for a few questions, he admitted he had no answers. And I told him I was going to create something called the Fauci rule. When you don’t know the answer to a question, don’t make it up. Just invoke the Fauci rule, which is named after your statement when President Biden took office that you would tell us if you don’t know an answer to a question. And I hope that using your name is OK with you.
ANTHONY FAUCI: That’s fine, Ira. Go ahead. It’s not good to guess when you’re dealing with public health measures.
IRA FLATOW: Yeah. And don’t you feel it’s very important for scientists when communicating with the public to say they don’t have all the answers?
ANTHONY FAUCI: Yeah. I mean that’s critical. I think people feel because they are representing science and science is knowledge that when they’re asked the question that somehow or other they have to give an answer. And one of the things that I’ve guided myself by is that if you really don’t know, just say you don’t know.
IRA FLATOW: Do you feel the level of progress in fighting COVID-19 over the last few months is now where you want it to be?
ANTHONY FAUCI: Well, certainly, the vaccines have been such an extraordinary success story over and above what we really anticipated. We were hopeful that we could quickly get a vaccine proven to be safe and highly efficacious and get it into the arms of people in a relatively short period of time. But what has been accomplished is really unprecedented and extraordinary. The sequence of the virus only being made public on January 10th and a phase I trial having occurred about 65 days later, a phase three trial on July 27th, and then vaccine literally in the arms of people by December.
That would have been something you and I, if we were having a conversation the way we used to years and years ago, we would have thought that this would be completely beyond the realm of reality. But it’s happened. And what it is, it’s an extraordinary testimony to the exquisite scientific advances that have been made not only in vaccine platform technology, but also in structure based vaccine design to get the spike protein in the right confirmation to be maximally immunogenic. All those things are a real testimony to science.
IRA FLATOW: How long do you think it will be before vaccinations will be available to everyone? I saw last week you said April and now I heard you say this week may be closer to May or June. Is it a moving target?
ANTHONY FAUCI: No. Actually, in some respects, it is. And the reason I kind of modified the statement, Ira, because I was hoping that when J&J, Johnson and Johnson vaccine came online, they have promised to have 100 million doses. And I was hoping we would get a substantial chunk of that in April. But that’s not going to happen. It likely will get few doses this month, maybe less than 20 next month, and then only after that will we start getting increased numbers.
So that’s the reason why I modified my statement saying I would have liked it to have been April where everyone can start getting vaccinated. Even if we start in April, which now I don’t think we will, by the time you get everyone vaccinated who could be vaccinated, that’s going to take several months. So it won’t be till the end of the summer before that happens.
IRA FLATOW: Does the federal government have any way to boost the number of vaccinations available or is it purely up to the drug companies about how many they can make?
ANTHONY FAUCI: Well, the government contracts, as we did with Moderna, and Pfizer, and J&J, and Novavax, and AstraZeneca, what the government can do, theoretically, if the vaccines are not being made quickly enough is to invoke the Defense Production Act, the DPA, which means that they could literally take over a factory or a company and say you’ve got to start making this vaccine.
The only problem with that, Ira, is that the process of making an mRNA vaccine is so complicated and so exquisitely sensitive that by the time you marshaled another company or another group to do that, we will already be into the realm of the spring and summer where we have the 600 million doses that we contracted for.
IRA FLATOW: Let’s talk about the variants that everybody has been talking about, like this listener Yung in California.
YUNG: I would like to ask Dr. Fauci about the strategy of our government and the scientific community with regard to the emerging virus variants, especially those which significantly change the shape of the spike and thus reduce the efficacy of the existing vaccines.
IRA FLATOW: What is the strategy for fighting these variants?
ANTHONY FAUCI: Well, the first thing you have to do, and we’re doing this now much more vigorously than we were before, is to intensify our genomic sequencing, namely sequence surveillance so we can see what is going on in the community, what mutants are evolving.
Let’s take a couple of examples that would answer the person’s question. So one of the ones that is dominating now in the UK and modelists predict, since it’s already here in the United States, that by the end of March it could be the dominant strain that’s circulating– and that’s the B117 strain, again, that originated likely in the UK.
That one, although it spreads more readily and is more transmissible, and recent data indicate that it could even be a higher degree of pathogenesis, the fact is that our vaccines do very well against it. It doesn’t evade the protection of the vaccine nor does it influence the capabilities of the monoclonal antibodies.
In contrast, the South African variant, the 351, that is different because that diminishes considerably the efficacy of certain of the monoclonal antibodies. And it also diminishes the efficacy of the vaccine. It diminishes it by multiple fold but it doesn’t take it below the threshold of efficacy. So the vaccines that we’re using now still are effective not as much against mild disease but quite effective against severe disease leading to hospitalization and death.
So what we’re doing about it besides surveillance is that we’re taking the first steps towards the possibility of having to upgrade the vaccine by making a booster shot that is reflecting and coding for the spike protein that represents the mutant as opposed to the wild type virus. So it’s surveillance. It’s the use of our own vaccine. And it’s the development of variants of the original vaccine.
IRA FLATOW: When you say, a booster shot, does that mean for everyone who got the first two shots, they would go back for a booster shot later?
ANTHONY FAUCI: That is conceivable. I don’t believe we need to do that now but we’re preparing for the possibility that we might. If it turns out that the variants totally dominate and the current vaccines don’t work, let’s say, a new variant that’s worse than 117, that’s worse than 351, then you might want to make a multivalent vaccine that is good against the wild type but also against the mutants so that you can essentially when you start to de novo vaccinate someone, you vaccinate them right from the get go with the mutant vaccine.
IRA FLATOW: And when do you make that decision? And who makes that decision to make the modified version?
ANTHONY FAUCI: Well, I mean we have a very strong relationship of a public private partnership with each of the six companies that the federal government has made a major investment in. We had Operation Warp Speed from the last administration that was responsible for putting together the plans to get these five or six vaccines developed and put into clinical trial. The equivalent of that is a leadership group that makes those decisions. So it’s a core group of public private partnership that makes that decision.
IRA FLATOW: Our listeners– a lot of them have questions about vaccines for children. Here’s one from Dean in Tucson.
DEAN: Where do we stand on inoculating children? Seems if we really want to open schools, everybody inside the building should be vaccinated– children, teachers, custodians, et cetera.
ANTHONY FAUCI: Well, ultimately, you obviously want to vaccinate all children similar to vaccinating children for the common childhood diseases as well as influenza. So let’s get that straight. We definitely want to do that. However, since children are vulnerable and generally don’t have informed consent for themselves, then you want to make sure the vaccine is both safe and effective in a normal adult population before you start vaccinating children. We’ve already proven that’s the case.
So what has started now, from a number of companies, particularly Pfizer, is to do an age deescalation study. In other words, taking children from 12 to nine, then nine to six, and then further down to show that the vaccine in a phase one and 2A trial is both safe and induces the kind of response that you would predict would be protective because it correlates with the response in those individuals who’ve gone through the efficacy trial. So you don’t have to do a 30,000 person trial for every age group of children. You could do it in a much smaller group of 1,000 just to show safety and to show immunogenicity. That’s going on right now. Likely, Ira, it won’t be until the end of the summer, the early fall where we do get to that point.
IRA FLATOW: Yeah. Our listeners alluded to schools reopening in person. And that is a big priority for the Biden administration, is it not?
ANTHONY FAUCI: Very much so. But to get the schools open, it isn’t a sine qua non. You don’t have to have all the teachers vaccinated and all the children vaccinated. Depending upon the degree of circulating virus in the community, you can get the kids back to school as long as you practice certain well-defined public health measures that are very clearly delineated in the recently published CDC guidelines for getting children back to school K to 12.
IRA FLATOW: This is Science Friday from WNYC Studios. Is there a special or one of the vaccines that you feel is going to be more effective in kids than the others?
ANTHONY FAUCI: No. We don’t know that yet, Ira, because we haven’t tested them in children. Right now the ones that we have an EUA for are the Moderna and the Pfizer product, the mRNA. Very soon, likely by February 26, the data from the J&J will have been fully evaluated by the FDA and their advisory committee will meet. And hopefully, we’ll see about getting an EUA for that product also.
IRA FLATOW: So many questions from our listeners about kids. Listener Carrie on Facebook wants to know if there’s any data so far about adverse reactions in children during these vaccine trials and, more specifically, if any epigenetic predispositions cause complications.
ANTHONY FAUCI: The answer is no and no. First of all, we are not aware of any epigenetic conditions that are issues with this type of a vaccine. The only experience now is that one of the companies that started off at 16 are now down to 12-year-olds so we do have some experience with 12-year-old but not yet with the 12 to nine and nine to six.
IRA FLATOW: Where are we at in terms of treatments? We’ve talked about vaccines. Now what about treatments for COVID-19? Anything new being tried out?
ANTHONY FAUCI: Well, there have been a number of studies, some of them placebo randomized controlled trials, that have shown efficacy, particularly in late disease. For example, glucocorticoids, dexamethasone was shown in a randomized placebo controlled trial in hospitalized patients on ventilators or requiring high flow oxygen that it diminishes significantly the 28 day mortality. Then there are others, such as monoclonal antibodies, mostly by the company Lilly and Regeneron, would show efficacy, particularly if given very early in the course of infection, to prevent you from requiring to be hospitalized.
Then there are a number of other studies- convalescent plasma, hyperimmunoglobulin. The thing that we really need, Ira, that would be really a boon to all of this would be a direct acting antiviral agent similar to what we developed for HIV, the antiretrovirals that so effectively were able to block virus replication, and the same type of thing we developed for hepatitis C in which we were able to cure hepatitis C with direct acting antiviral agents. There are a number of companies working on that. We are very interested in pursuing those types of studies.
IRA FLATOW: We got an interesting question from Ethan in Middlebury, Indiana.
ETHAN: Most of the population has made efforts to reduce the spread of COVID-19. How do you see this affecting other transmissible diseases both currently and longer term?
ANTHONY FAUCI: Well, that’s a great question. And we also have some really good information on that. During our summer when we were getting hit really badly, and we still are getting hit very badly with COVID-19, our colleagues in Australia who were going through their winter, which would have been their flu season, contacted me and said, Tony, you’re not going to believe it but we are virtually seeing no influenza. This is the first time in all of our years of experience when there were so few cases you could barely count them. I mean, just virtually none. They were suspicious that, because of the public health measures, the masking, the washing of hands, the avoiding congregate settings, the keeping physical distance might be preventing them from getting flu, paraflu, respiratory syncytial virus.
Sure enough, in our winter, which we are now well into our winter in February, we’re seeing the same thing. We’re seeing hardly any influenza and hardly any of the other respiratory infections that we always see spike in the winter, which tells you that those public health measures of washing your hands, physical distance, masking, those types of things really work.
IRA FLATOW: We have to take a break. And when we come back, we’ll continue our conversation with Dr. Anthony Fauci about COVID-19, vaccines, and a new normal. We’ll be right back. This is Science Friday from WNYC.
This is Science Friday. I’m Ira Flatow. We’re continuing our conversation with Dr. Anthony Fauci about COVID-19 vaccines and returning to a new normal. So many people out there have been separated from their families and their friends for almost a whole year now, as you know. And now that more people are getting vaccinated, there is a glimmer of hope out there. At what point do you think it’s OK for two people to see each other in person and share a meal and a hug for example? Should both parties be vaccinated? Is one party vaccinated enough? What’s the ruling on that?
ANTHONY FAUCI: Well, I like the last part of your question, Ira, because there is no ruling yet. But what will happen is that as we get more and more people vaccinated that we’ll have to, if we don’t have hard data, make some common sense type recommendations.
For example, if you have three members of a family, a husband, a wife, and a child who lives in a different city, prior to getting vaccinated, if you wanted to see your daughter or your son who would come into town, they would have to quarantine themselves for a certain period of time, likely get tested, wear a mask when you’re with them, and only then feel comfortable. Well, right now, if all three of those people are doubly vaccinated, common sense tells you that the relative risk is really, really low when all three are doubly vaccinated.
So people are going to start realizing that the relative risk is low and will likely be able to say, you know, come on down. Travel. Come into the house. You don’t have to quarantine. You don’t have to wear a mask. And I’m going to give you a big hug. I think that’s going to happen. But I don’t think there’ll be a formal recommendation of that until we get a very large proportion of the population vaccinated.
IRA FLATOW: And you’re saying that’s for when you come into the house to give somebody a hug. But if you’ve been vaccinated and you’re still out in the public, doesn’t that still mean because there could be virus still in your nose, you could still spread it?
ANTHONY FAUCI: Absolutely. So what I’m saying is that there are things you can do in your own pod, in your own family unit. Then that changes when you talk about how you act in society when the vast majority of people are not vaccinated and you might have virus in your nasal pharynx because you got infected and the vaccine didn’t protect you against getting infected, but it did protect you against getting ill, that you could conceivably spread it to somebody else, which is the reason why when you’re outside of your own private family pod that you’re going to act a little bit differently than you do in your own closed circles.
IRA FLATOW: OK. So I guess the $64 question is what is the metric for knowing when we can all return to normal? How will we know that?
ANTHONY FAUCI: I don’t think you’re going to definitively know it, but you can get a pretty good guess. When you get the overwhelming majority of the population, and I would say 70% to 85% of the population vaccinated, and the level of infections per day in the community are so low that they’re not even close to being considered a threat. Right now, even though the numbers of infections are going precipitously downward, we still have 60, 70,000 infections a day. We were up to 300 to 400,000 a day just a few weeks ago. When you get that level of viral in the community very low, then you could start thinking of returning as a society to some form of normality.
IRA FLATOW: Let’s talk about the possibility of creating a single vaccine for all coronaviruses. Carl Zimmer writing in The New York Times talks about past efforts to develop a universal vaccine that were stymied by loss of government funding.
He writes, quote, “Dr. Matthew Memoli, a virologist at National Institute of Allergy and Infectious Diseases”– your place– “looks back at those decisions as an enormous blunder. It’s a failure of our system of science, he said. Funders tend to chase after shiny objects.” Let me ask you. In hindsight, were there missed opportunities here?
ANTHONY FAUCI: No. I think maybe Matt got a little carried away there. The fact is that we have made major investments in the development of universal flu vaccine. And we’re making major investments now in a universal SARS-CoV-2 and then ultimately coronavirus vaccines in general. We definitely are committed to that and we have for a very long time.
IRA FLATOW: I first began talking with you about disease way back in the early 1980s when HIV/AIDS was quickly emerging. Do you think we will have an AIDS vaccine any time soon? And wouldn’t it be a fitting way coming full circle for a way for you to retire finally?
ANTHONY FAUCI: You trying to get rid of me, Ira?
IRA FLATOW: Never.
ANTHONY FAUCI: So vaccines, as we’ve discussed on your show more than once, Ira, vaccines for HIV are really problematic for the simple reason that the body does not like to make an immune response against HIV that is an adequate response to clear the virus and maintain essentially protection for life. Until we figure out a way to get a vaccine to do better than natural infection in inducing the kind of response that would be protective, we’re not going to have an effective HIV vaccine.
Do I think that’s impossible? No. I think we’ve just got to use all of our scientific tools of structure-based vaccine design, of putting that envelope trimer in the right confirmation to trigger broadly neutralizing antibodies. I believe that when that occurs, we’ll get a vaccine for HIV.
IRA FLATOW: Listener Arianna on Facebook wants to know, what possible medical and scientific breakthroughs do you think we’ll see from all this research focused on COVID-19 and mRNA vaccines?
ANTHONY FAUCI: I think it’s going to open up a whole new avenue of approach to vaccines. You might recall, I do certainly, that when we put an investment in the mRNA vaccines, there was a lot of concern if not criticism that why are you making investment in vaccines that have never resulted in a marketable vaccine before when we have such a serious problem.
Well, as it turns out, it’s been a roaring success. And we’re already starting to see people trying to apply the lessons and the technologies not only of the platform technology of mRNA but also of the structure-based vaccine design the same way as Barney Graham showed that the stabilization of the prefusion spike protein was very much more immunogenic than the post-fusion conformation.
IRA FLATOW: One last question for you, because when I look at all the conversations we’ve been having about vaccines, now mRNA, spike proteins, immunity, all of it, people are getting an education in biology that they never got in school before. We’re talking about stuff that never would have been a topic of discussion. Do you ever feel that way, that we’re having a giant class here?
ANTHONY FAUCI: Very much so, Ira. And that’s the beauty of what’s going on right now is that science is evolving so rapidly. And we’re seeing the fruits of fundamental basic science. And you’re able to just show and demonstrate these biological mechanisms that are responsible for real world results. I mean I think the development of a highly efficacious vaccine by a new platform together with structure-based vaccine design of the immunogen is just exactly what you say. It’s a lesson in biology.
IRA FLATOW: Thank you, Dr. Fauci.
ANTHONY FAUCI: Always good to be with you, Ira. Thank you for having me.
IRA FLATOW: You’re welcome. Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases in Bethesda, Maryland, and a recipient of the Presidential Medal of Freedom.
Copyright © 2021 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Kathleen Davis is a producer and fill-in host at Science Friday, which means she spends her weeks researching, writing, editing, and sometimes talking into a microphone. She’s always eager to talk about freshwater lakes and Coney Island diners.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.