Anthony Fauci Reflects On 40 Years Of HIV/AIDS Research
28:03 minutes
 Do you want to go back in time with SciFri? Sign up for the Science Friday Rewind newsletter to get more never-before digitized stories and audio bites from our archives!
Do you want to go back in time with SciFri? Sign up for the Science Friday Rewind newsletter to get more never-before digitized stories and audio bites from our archives!
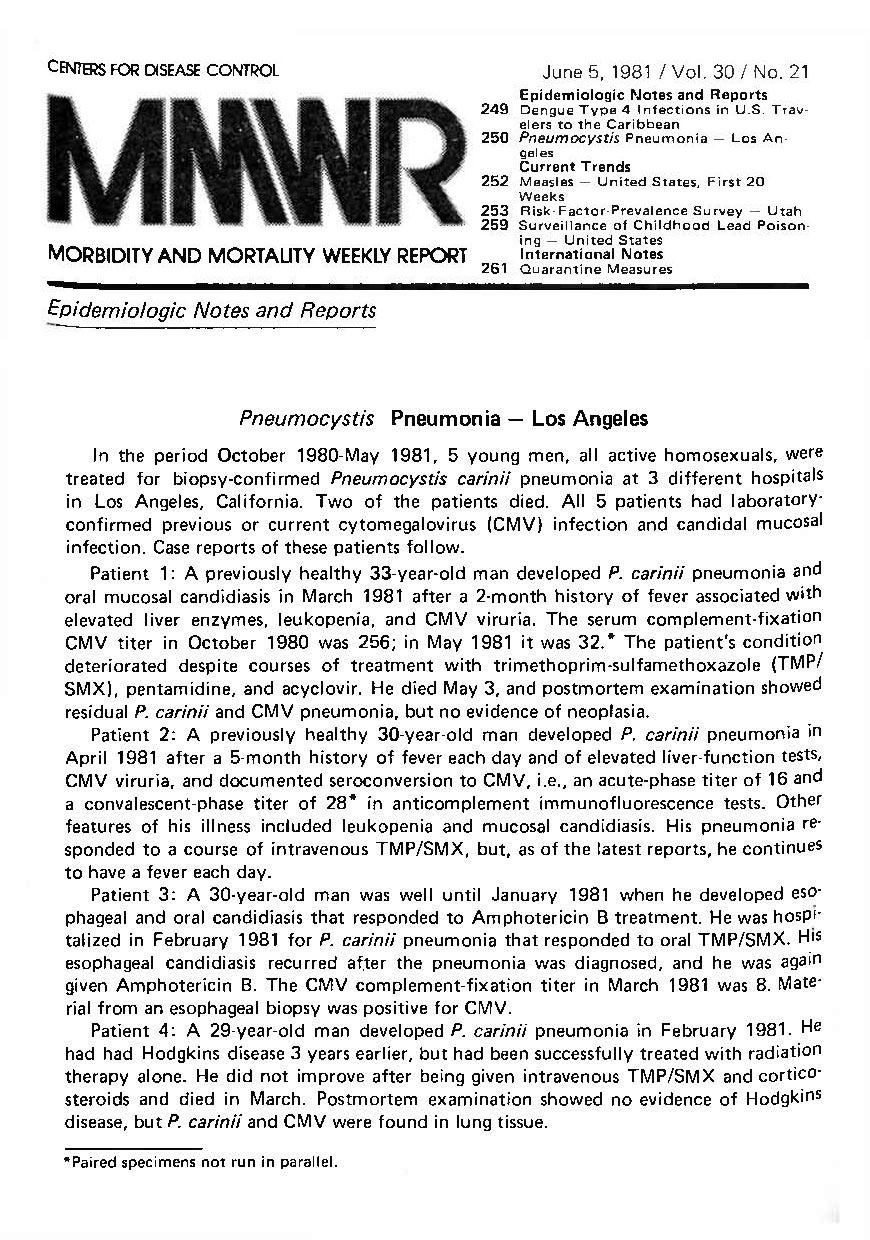
Every week, the Centers for Disease Control and Prevention (CDC) releases its regular report of the latest developments on emerging diseases—a living record documenting decades of medical history, known as the Morbidity and Mortality Weekly Report (MMWR). In May 1981, former MMWR editor Michael B. Gregg got a call about an unusual deadly pneumonia, seen in young gay men in Los Angeles. The tip was from epidemiologist Wayne Shandera, Epidemic Intelligence Service Officer for the Los Angeles County Department of Health. He described the cases of five men, ages 29 to 36, who had developed Pneumocystis carinii, a kind of pneumonia typically seen in cancer and immunosuppressed patients. These men were previously healthy, yet they struggled to fight off the illness with treatment. Two of the patients died. All five were gay.
Gregg didn’t know what to make of the cases, but he and CDC experts were compelled to publish the observations in the June 5, 1981 issue of MMWR. Soon after, clinicians around the country began to flag similar cases. The number of infected people rose, as did awareness of the strange collection of symptoms. That summer, the media ran stories about the mysterious disease; the New York Times published the headline, “Rare Cancer Seen in 41 Homosexuals.” At that time, Ira was a science correspondent for NPR, and was in the thick of covering the nuances of the illness:
Today marks 40 years since the first official report on the HIV/AIDS epidemic in the United States, and the beginning of a long-puzzling medical mystery. “I was totally baffled, and did not know what was going on. I thought it was a fluke,” recalls Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, during an interview this week with Science Friday.
“I made a decision literally when I was reading that horrifying MMWR,” he says. “I had never seen anything like this in otherwise healthy young people. And I said, ‘I’m going to change the direction of my research. And I’m going to study these young gay men who have this terrible disease.’”

Since the 1981 report, nearly 33 million people have died from AIDS-related illnesses. But over the last four decades, preventative healthcare and treatment options have helped reduce transmission. The development of various drug cocktail treatments and therapies have become effective enough for people with HIV to live long lives. This disease has undoubtedly changed the way the medical field approaches immune dysfunction, and has left a lasting impact on American culture.

Despite this progress, the HIV/AIDS epidemic continues. Thirty-eight million people worldwide currently live with HIV, as of 2019 data. Infection rates have declined among white gay men in big cities who were initially hit the hardest; the virus now disproportionately affects Black gay and bisexual men in the American South. The health crisis has deepened medical, cultural, and societal divides across the world—mirroring the disease disparities in Black, Latino, and Native American communities during COVID-19.
In an interview with SciFri in June 2020, Fauci reflected on the similarities between the uncertainty of the COVID-19 pandemic, and the HIV/AIDS epidemic. “There’s so many things that are analogous to what was going on when [we] were talking about it back in the early ’80s—the mysterious nature, the protean manifestations of disease,” Fauci said. “The more we learn about it, the more we realize how little we know.”
In 1982, the CDC made its first mention of “acquired immune deficiency syndrome,” or AIDS, to classify the cases. By then, there had been nearly 600 cases of infection and 243 deaths. “There’s no question that it’s an epidemic,” Dr. Alvin E. Friedman-Kien, a dermatologist in New York City, told Ira for NPR’s All Things Considered on April 20 of that year. “But the question that one asks is: Why has this disease not been seen before? Why is it occurring now? And why is it occurring among this particular group of individuals?”
The initial outbreak of AIDS in the United States was largely seen in gay communities in urban centers, and later associated with drug users. The unknowns of the disease bubbled up discussions about sexuality, illicit drug use, and sexually transmitted diseases—conversations that many considered taboo in the 1980s and early 1990s. Society and the media wielded insensitive language that often blamed and alienated the gay community. When a patient tested positive for HIV, they not only had to battle a life-threatening disease, but the stigma that came with it.
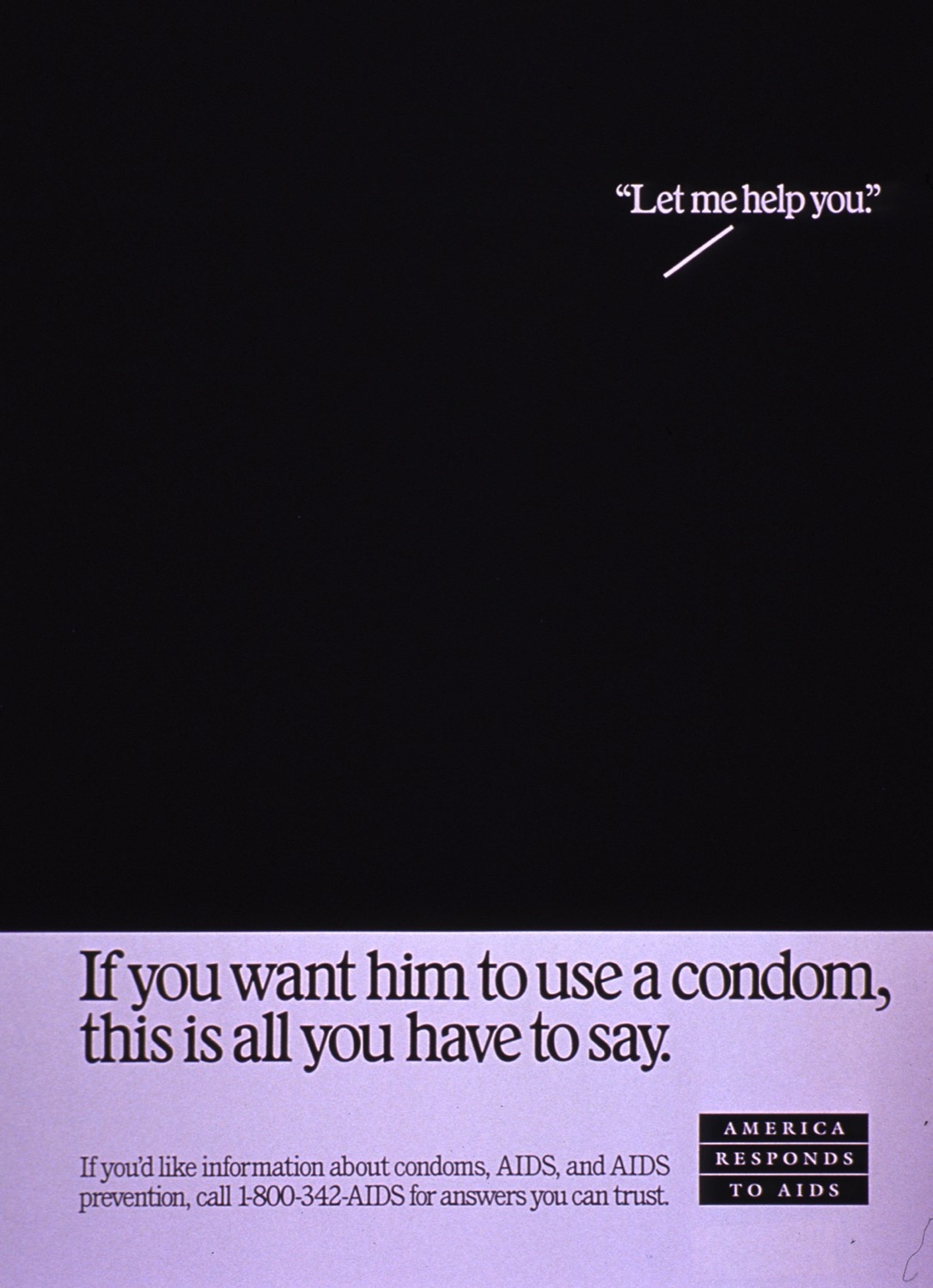
The week of Science Friday’s first broadcast on November 8, 1991, basketball icon and household name, Earvin “Magic” Johnson, publicly announced that he had tested positive for HIV. “I think sometimes we think, ‘Well, only gay people can get it, and it’s not going to happen to me.’ And here I am saying that it can happen to anybody,” he said on November 7. The news shocked the public, and left many divided. In the second hour of our very first show, we covered Johnson’s announcement, with dozens of callers voicing their opinions.
“I think it’s a little bit disingenuous when people react and the media reacts and politicians react like this is brand new news,” said one listener in San Francisco. Another caller who was an HIV patient, also from San Francisco, expressed frustration over the sudden shift in tone and attention from the public and media when “someone who is held up in public esteem as some kind of hero and idol” contracts the disease. “I admire him for the courage that he had yesterday in doing this, but there are heroes that have been fighting this goddamn war for the last 10 years. And they don’t get recognized.”
Magic Johnson’s pledge to fight the disease, and his vocal support towards education about it were an “important” turning point in the public’s perception towards AIDS and HIV, Fauci says in our recent SciFri interview. Johnson’s announcement opened up conversations about sex and sex education, and changed ideas of who were at risk of getting the disease.
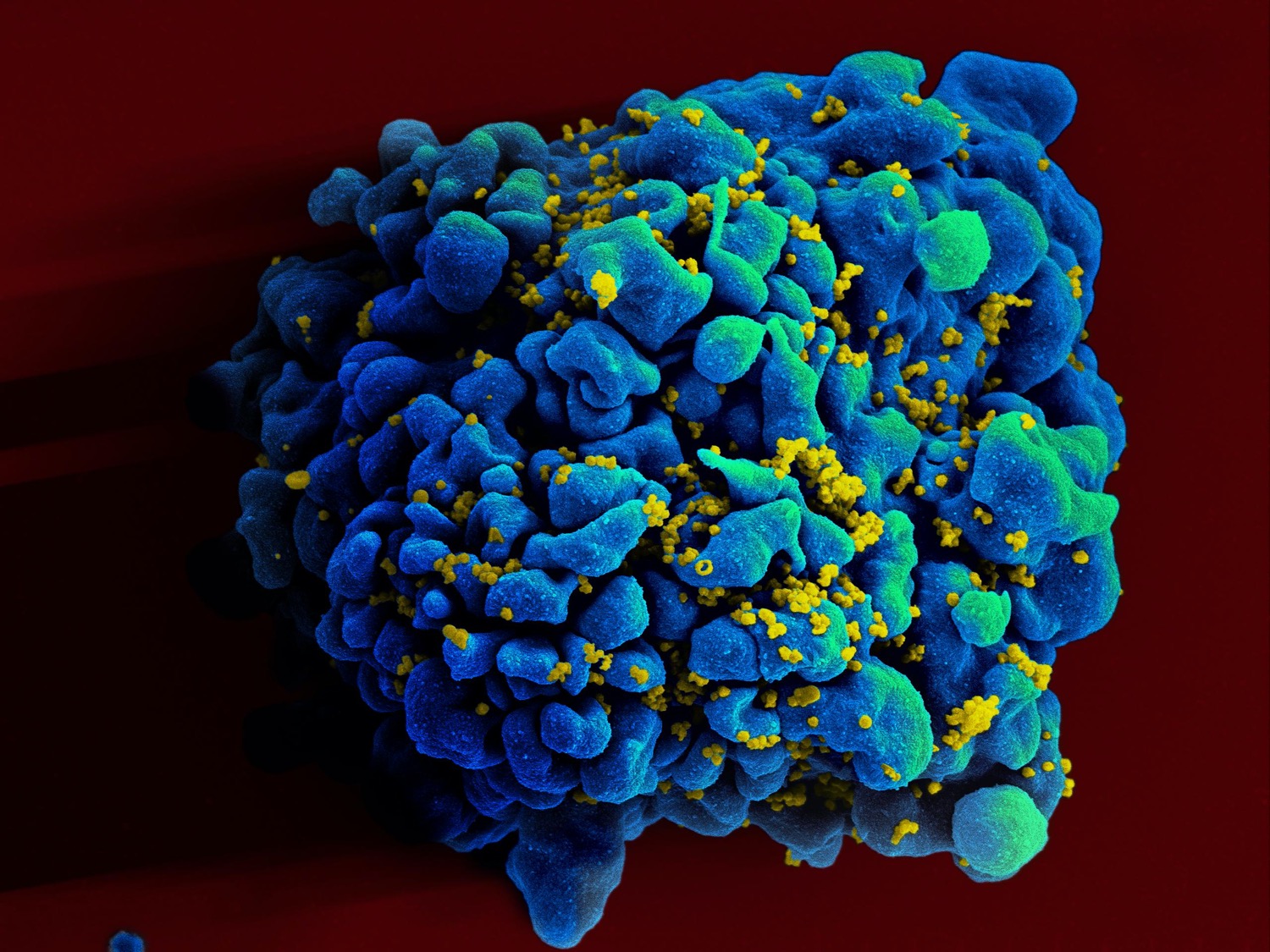
In one of his first interviews on the show in 1994, Fauci described HIV as a “formidable foe,” an elusive invader for the immune system to fight off. The virus is able to weave its genetic material within human genes—covertly becoming a part of the cell it infects, and making it difficult for drugs to target. Back in 1994, Fauci explained that scientists first had to understand the “fundamental basics” of how the virus compromises the immune system in order to find effective treatment, therapies, or a future vaccine.
“As time goes by, we do understand more and more,” Fauci said in 1994. “The answer may not be around the corner, but the scientific advances come in a very stepwise fashion that don’t sound sexy, as it were, so people can read in the newspaper, ‘Wow, what a big, great advance this is.’ But it does take scientists and the science enterprise closer and closer to what the ultimate goal is.”
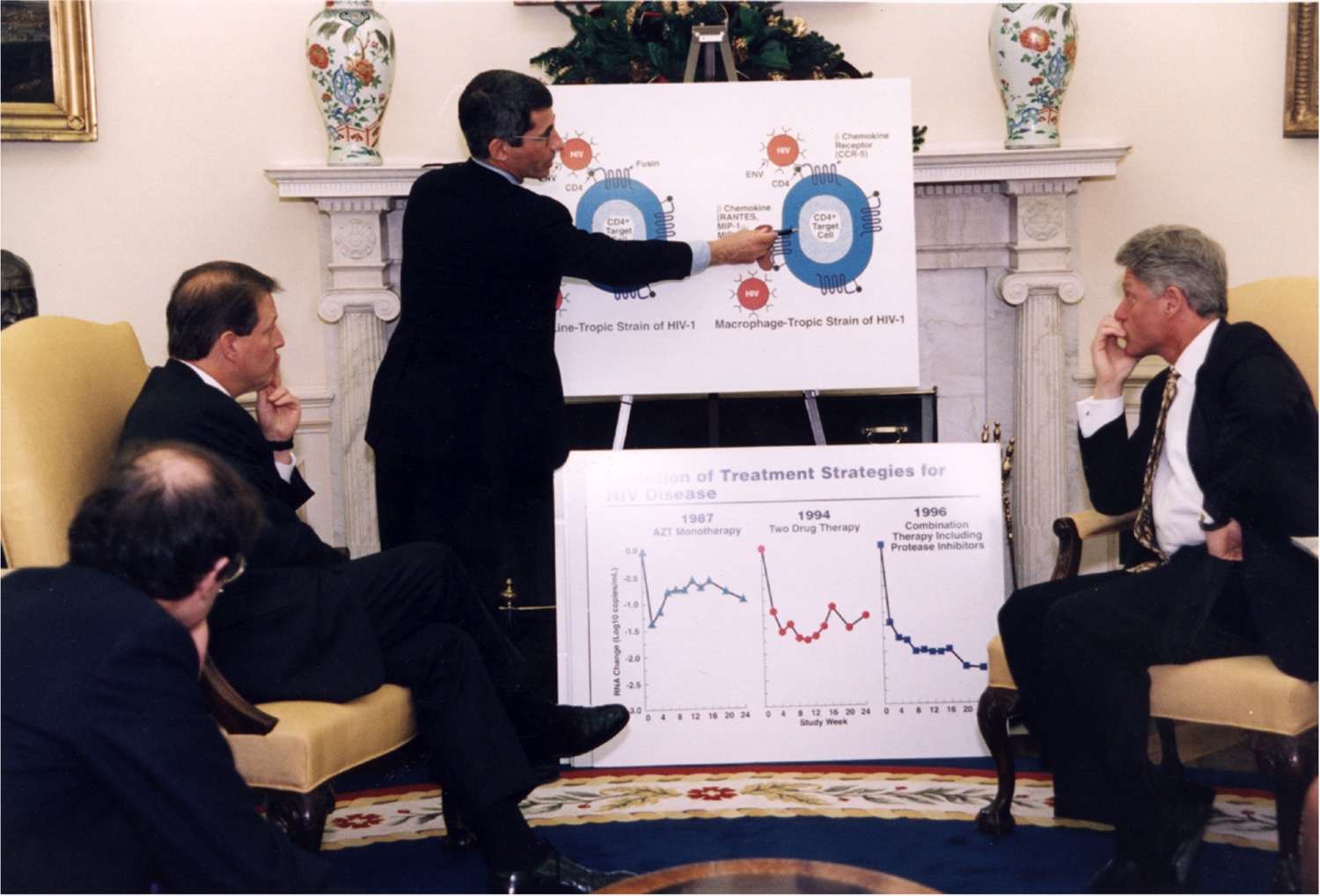
A flurry of research and policy changes in the 1990s and early aughts led to a better understanding of the virology of HIV, a retrovirus which infects specific cells in the human immune system and can deplete CD4+ T cells, causing AIDS. As scientists understood more about how the virus attacks and the clinical presentation of AIDS, they were able to develop tools like accessible testing, more effective active antiretroviral therapy (HAART), and the approval of Truvada for pre-exposure prophylaxis (PrEP). Over time, this has turned HIV/AIDS into a treatable, chronic illness for some patients.
But communities that lack this essential care continue to struggle with the HIV/AIDS epidemic. The disease is a serious public health issue in many parts of Africa, Asia, and Latin America, while pockets of the United States also still see spikes in cases: “In some areas of the country, particularly in rural areas of the South, which are demographically overrepresented with African Americans, the stigma, the lack of access, all of those other factors have made it very difficult to have that kind of accessibility to all the things that you need to really stop the outbreak,” Fauci tells SciFri this week.
In 2019, the CDC reported that more than half of new HIV diagnoses in the U.S. happened in southern states, with African American men making up a disproportionate number of those cases. There are many factors driving the South’s HIV/AIDS epidemic, as Fauci explains—poverty, unemployment, lack of transportation, and not qualifying for health insurance all contribute to poor health outcomes. This inequality of care continues to be a challenge in combating infectious disease outbreaks today.
Despite those systemic failures, other lessons from HIV and AIDS have proven helpful in furthering drug and vaccine development for other diseases. While scientists have still been unable to successfully create an HIV vaccine, the four decades of research and technology helped accelerate the development of the COVID-19 vaccine, Fauci says this week. “It seems a little paradoxical,” he says. “The types of elegant science that has evolved in an attempt, albeit thus far unsuccessful, to develop an HIV vaccine are technologies that have paved the way for the spectacularly successful COVID-19 vaccines.”
Still, Fauci is optimistic that COVID-19 vaccine research can pay it forward. “There are many HIV vaccinologists who are looking very closely at that platform technology to see if you apply the mRNA approach to HIV.” Fauci says. “I hope that what we’ve done with COVID-19 will help HIV.”
Find more SciFri stories and information—past and present—about HIV and AIDS below. And check out more archival stories from Science Friday Rewind.
Archival interview excerpts have been edited for length.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Anthony Fauci is the former Director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health, and author of On Call: A Doctor’s Journey in Public Service. He’s based in Washington, DC.
IRA FLATOW: This is Science Friday. I’m Ira Flatow.
SPEAKER 1: My best friend that died of Kaposi sarcoma was the second case of it in New York.
SPEAKER 2: I have five, six friends, now, who have died. And I have four or five other friends who are in chemotherapy. And these are all guys who are in their 20s and 30s.
IRA FLATOW: Voices from a different era, a different illness. I bring up those voices from a story I covered for NPR’S All Things Considered 40 years ago because Saturday, June 5th marks the 40th anniversary of a major medical milestone. On that day in 1981, the CDC published a report of a strange occurrence. Five young, otherwise healthy men in Los Angeles were hospitalized for pneumocystis pneumonia. This pneumonia is an illness that normally strikes seriously ill patients whose immune systems have been compromised.
But these young men confounded doctors because, for all intents and purposes, they should have been able to fight off this sickness. Two of these five men died. But they all had one thing in common. All five were gay, and this report kicked off a long head-scratching few years where the medical community could not figure out what was happening to mostly gay men who lived in cities. Here’s a clip of mine from Morning Edition in 1981, right when this was emerging.
Something baffling is going on in major gay communities around the country. It’s a medical mystery more difficult to solve than Legionnaires’ disease. Homosexual men are succumbing to fatal diseases that they should normally be immune to. The news first became public last summer when the Center for Disease Control in Atlanta began keeping track of the outbreak of two diseases, pneumocystis pneumonia and Kaposi sarcoma, in young homosexual men in Los Angeles and New York.
It was a confounding and fearful time for a lot of people. Medical professionals couldn’t figure out what was going on. They didn’t know how it originated or spread. And gay communities in big cities were being decimated. The death rate for this mysterious illness was about 30%.
SPEAKER 1: To think, out of a community as big as they are, there are 180 or 190 cases or whatever it is. I know, personally, about eight of them. It’s an incredible when you think about it.
SPEAKER 2: You can’t not but be scared by all of that.
IRA FLATOW: Over the past 40 years, we’ve learned a lot more about HIV and AIDS. Treatments are readily available, and they work well, and the illness is no longer a death sentence. Joining me to reflect on this time is someone who was there from the beginning, Dr. Anthony Fauci, recipient of the Presidential Medal of Freedom and director of the National Institute of Allergy and Infectious Diseases in Bethesda, Maryland. Welcome back to the show.
ANTHONY FAUCI: It’s good to be with you as always, Ira.
IRA FLATOW: Listening to those clips, hearing that history, it’s got to evoke memories for you, Dr. Fauci.
ANTHONY FAUCI: Ira, it invokes very painful memories, having lived through that, literally, from the very first day that the first cases were reported in June of 1981 in MMWR. And I was totally baffled and did not know what was going on. I thought it was a fluke. And then one month later in July of 1981, it was a similar report only now of 26 curiously, very curiously, all young, gay men who now were not only from LA but from San Francisco and New York City who were now very ill not only with pneumocystis. But some had other opportunistic infections as well as Kaposi sarcoma.
And I made a decision, literally when I was reading that horrifying MMWR, because I knew that my entire professional career following my residency– I was about eight or nine years following my chief residency– I was seeing all sorts of infectious diseases. And I had never seen anything like this in otherwise healthy young people. And I said I’m going to change the direction of my research. And I’m going to study these young gay men who have this terrible disease that they’re presenting with far advanced immunosuppression and opportunistic infections.
And the years that I did that before we developed adequate therapy were really personified by the clips that you just played. I mean, those are the things that, even though they were 40 years ago, 39, 38 years ago, they resonate in my ears because I was there on the ground when it was happening, desperately– as some of my other colleagues were trying to do, be they in San Francisco, LA or New York– were desperately trying to find solutions which were elusive because we didn’t even know what the etiology was of this devastating disease among mostly young gay men.
But as the weeks and months went by we found out that it was not only young gay men, it was injection drug users and sexual partners of individuals who were infected. It was a terrible, terrible time, Ira.
IRA FLATOW: And at what point did it become apparent that HIV was passed through blood and bodily fluids?
ANTHONY FAUCI: Well, it was certainly apparent when very soon, and even before we identified the virus now known as HIV-1, that it was clear to us from a pure epidemiological standpoint that it was transmitted by blood, blood products, and to hemophiliacs through plasma derivatives because we were seeing this unusual situation where, wait a minute, we’re having gay men who clearly were in the middle of the sexual revolution with the bathhouse culture which is the perfect setup for the spread of a sexually transmitted disease.
And then you have people who are transfusion recipients. And then you were having hemophiliacs. And they were all getting infected. I mean, it wasn’t very difficult to put two and two together to know what we were dealing with. We just didn’t know what the etiologic agent was.
IRA FLATOW: I recall that a word that was thrown around a lot in those early days was baffling. Accurate description?
ANTHONY FAUCI: Yeah baffling and painful and dark. The only thing that really got us through was the extraordinary bravery of the young men who were going through an unprecedented, very frightening experience.
IRA FLATOW: A big day in the history of HIV/AIDS was when Magic Johnson told the world that he was HIV positive. The following is from the press conference he gave announcing his status in November of 1991.
MAGIC JOHNSON: Because of the HIV virus that I have obtained, I will have to retire from the Lakers today. I just want to make clear, first of all, that I do not have the AIDS disease, because I know a lot of you want to know that, but the HIV virus. I plan on going on living for a long time, bugging you guys like I always have. I will now become a spokesman for the HIV virus because I want people and young people to realize that they can practice safe sex.
And, you know, sometimes you’re a little naive about it. And you think it could never happen to you. You only thought it could happen to, you know, other people. And so on and on. And it has happened. But I’m going to deal with it. And my life will go on.
IRA FLATOW: Do you think this was a turning point for how people looked at other people with HIV?
ANTHONY FAUCI: Oh yeah. I think that whenever you get a celebrity who’s highly admired, almost universally, in the community– certainly Magic Johnson with that infectious smile of his and his exploits on the basketball court had many, many admirers– when you see someone like that who’s now living with HIV, the stigma associated with HIV is, I think, markedly diminished because people can identify very closely with someone they’ve admired for years.
IRA FLATOW: Yeah because, if I recall correctly, up to that point, a lot of people saw this as, quote unquote, “a gay disease.” And the community was sometimes vilified for this. I mean, remember there was a time when people were referring to AIDS as gay cancer.
ANTHONY FAUCI: Right, or gay-related immunodeficiency. GRID, that was the name that was used, right.
IRA FLATOW: And that sort of turned it around when Magic Johnson came out.
ANTHONY FAUCI: Indeed. Indeed, that was important.
IRA FLATOW: We talked about HIV on our very first Science Friday show back in 1991 in November. I want to play a comment from a caller from that show who summed that up very well.
AUDIENCE: I think it’s a little bit disingenuous when people react and the media reacts and politicians react like this is brand new news when something like this happens or, you know, a Rock Hudson or a Ryan White. And there’s this hidden level, I think, that, you know, this can happen to, quote unquote, “innocent” people. And the guilty people who are in the millions are right around the corner.
IRA FLATOW: Do you think, Dr. Fauci, that people could have done a better job to not villainize the gay community and drug users?
ANTHONY FAUCI: Oh, I mean, obviously. I mean, that was the stigmatization of a community that was disenfranchised from the beginning because of the levels, in various segments of our society, of homophobia. Then you superimpose upon that a mysterious, baffling illness. And then you associate that. Well, people who have injection drug use get it and commercial sex workers.
So what became villainized, instead of the virus, was, in many respects, the people who were afflicted with the virus, absolutely.
IRA FLATOW: Was research side-tracked at all by public perception?
ANTHONY FAUCI: Well certainly not those of us, myself and my colleagues, who jumped on this from, literally, the very first day. I believe that– and again there’s a lot of differences of opinion of that– but I believe if– well, President Reagan, with many of his good qualities, if he had used the bully pulpit of the presidency in a more proactive way to call attention to this, there would have been, A, more resources.
And with more resources, perhaps we would have done faster, more quickly, in some of the development of countermeasures. But also if there is a real show of genuine empathy on the part of the leadership in the country that may have gone a long way to have the rest of the country diminish the stigma associated with this disease.
IRA FLATOW: Was there a decision made by you and your office about which direction to take in fighting the illness, whether to develop a vaccine or to develop a treatment first?
ANTHONY FAUCI: Well, I think it was both done simultaneously, Ira. And one of the things that was the stumbling block of the development of a vaccine is that the body does not seem to want to or like to make a good immune response against the virus. So if natural infection itself does not induce an adequate immune response, one of the tenets of vaccinology is that the best way to get a good vaccine is to mimic natural infection without hurting the host. That’s the fundamental strategy of what vaccines are.
The only trouble is, natural infection itself does not induce an adequate immune response. Whereas when you look at other really serious diseases, like polio or measles or smallpox, as serious as they are for many people, in general, most people recover from this infection because they develop a very potent immune response that ultimately clears the virus and renders them protected from reinfection with the identical or very similar virus. That is what’s called nature providing you with the proof of concept of what the body can do.
Unfortunately we have no proof of concept that way with HIV vaccine. So we have to do better than what natural infection does. And that’s a very, very high bar for a vaccine. Whereas with therapeutics, you have the virus in hand, and you do targeted drug development by identifying the vulnerable targets in the HIV replication cycle. And you develop and target your therapies for those vulnerable targets, hence reverse transcriptase inhibitors, protease inhibitors, integrase inhibitors, fusion inhibitors. Those are the things that were developed.
And ultimately we developed combinations of drugs that were spectacularly successful in suppressing the level of virus so that people living with HIV can actually think about leading a normal life that’s almost with the normal life expectancy as well as knowing that if they remain undetectable that undetectable equals transmittable. So you’re not going to be a danger to anyone else. So there was really a very large dichotomy between what we have done and we’re able to do with therapies versus the success with a vaccine, for the reasons that I just mentioned.
IRA FLATOW: This is Science Friday from WNYC Studios. In case you’re just joining us, we’re talking to Dr. Anthony Fauci about what we’ve learned over 40 years of HIV/AIDS research. Did you learn anything– and I don’t mean you in particular, although it might be you– any lessons from the COVID episodes we’re hopefully getting out of that might be applied to HIV or vise versa? Did we learn anything from HIV that might be applied to combating COVID or future cases of this?
ANTHONY FAUCI: Well right now that there’s no doubt that the types of elegant science that has evolved in an attempt, albeit thus far unsuccessful, to develop an HIV vaccine are technologies that have paved the way for the spectacularly successful COVID-19 vaccines. It seems a little paradoxical that technologies, structure-based vaccine design, getting the right, stable conformation of a particular immunogen, are all things that originated out of work with HIV that has been applied to developing the right prefusion component that stabilized of the spike protein that is a wonderful immunogen for COVID-19 and has led to vaccines with up to 94%, 95% efficacy and even better in effectiveness in the real world.
Yet that same technology has not delivered for us an HIV vaccine. Now that we have this highly successful mRNA platform technology, there are many HIV vaccinologists who are looking very closely at that platform technology to see if you apply the mRNA approach to HIV, will we be able to make some giant steps towards a vaccine. So even though it’s gone one way, namely HIV helping COVID-19, maybe, and I hope, that what we’ve done with COVID-19 will help HIV.
IRA FLATOW: We have to take a quick break. And when we come back, we’ll have more with Dr. Anthony Fauci about the 40 years of HIV/AIDS. We’ll be right back. Stay with us. This is Science Friday from WNYC Studios.
This is Science Friday. I’m Ira Flatow. We’re continuing our conversation with Dr. Anthony Fauci about 40 years of HIV and AIDS in the US, how much we’ve learned, how much is still unknown about the illness that was so frightening four decades ago. I want to play a clip from another Science Friday show 26 years ago, back in 1995. You were on the show with Bob Gallo who co-discovered that HIV was the virus responsible for AIDS.
And in this show we talked about the latest HIV/AIDS treatments that had been discovered and discussed all the things we still don’t know about the virus, this was 26 years ago. And I brought up the point that it seemed like there’s a lot we don’t know about the human immunity system and how HIV plays into it compared to how much we know about other systems in the body. And that got some pushback from both of you.
Bob Gallo, does this mean we really don’t understand the human immunity system that well?
ROBERT GALLO: Very often, scientists will say we don’t know anything, we don’t know much, we’re just scratching the surface. I feel on a relative scale, we know quite a bit about HIV relative to other viruses. And I think the field of immunology is a rather well-developed field. However, you can make the argument either way. If somebody says we know nothing, you can argue that’s ridiculous. You can say we know an awful lot. You can say the same thing. But being more the virologist, I’d rather punt that right to Dr. Fauci.
ANTHONY FAUCI: Well, you know, I take issue. I take issue with the point that was made that we know everything about all of the other systems but we don’t know much about the immune system. I disagree strongly with that. I mean if you look at the neurological system, of which we know a lot, there are more mysteries in the neurological system than you could even imagine. And in the endocrine system, a variety of systems, I don’t think the immune system is any much further off in the amount we understand or don’t understand.
I think the point that Bob made is a very good point. And I think that’s the reason why there’s a lot of confusion. We an awful lot about HIV. We know how the virus works. We know how the virus destroys the body’s immune system. But we don’t know everything. And that’s the reason why the kinds of discovery that was made by Bob and others most recently adds more to the store of knowledge.
But to say that we know very, very little about it, I think, is overexaggerating. Or to say that we know everything is certainly a naive oversimplification. We’re making step by step progress. There’s a ways to go. But we do know an awful lot about it.
IRA FLATOW: First of all, Dr. Fauci, it’s great to be reminded that you’ve been a straight talker for all of these years and not afraid to speak your mind. In hindsight, did we know a lot about HIV at this time?
ANTHONY FAUCI: Yes, we did an awful lot about it. One of the things that as the years went by, Ira, that really was, I would say, a little bit disturbing if not quite disturbing was that the full realization that when you present the antigen and the form of an envelope, trimmer, or whatever mechanism you’re using in your vaccine platform that the body doesn’t make broadly neutralizing antibody. And when you have a virus that continually mutates and changes because of the pressure of the immune system then you’ve got to get antibodies that are broadly neutralizing to all iterations of the virus.
When you get a disease like measles, measles doesn’t change a heck of a lot over decades, much less within a person over a period of months to years. So that’s why– you just need antibodies against the appropriate component of the virus to block it. That was the thing that we still don’t know yet, Ira, exactly how to induce broadly neutralizing antibodies against HIV.
IRA FLATOW: Are we getting any closer?
ANTHONY FAUCI: We are. And I think we’re getting closer because we’re using very sophisticated technology of structure-based vaccine design, whereby using cryo-electron microscopy and looking at the right confirmation that would, in fact, trigger the B cell lineage so that you can actually trigger the appropriate lineages to coax it along to get to the point of making broadly neutralizing antibodies. That might require an approach to vaccinology that we’ve never had to do before, is to give sequential immunizations with a modified form of the immunogen to continue the pathway to broadly neutralizing antibodies.
IRA FLATOW: So you’re saying just constantly giving people booster shots.
ANTHONY FAUCI: Well, yeah, sort of. I mean, a version of a booster shot where you bring it to one point in differentiation and then you bring it to the next so that you get to the point where you really do have broadly neutralizing antibodies.
IRA FLATOW: And how far along are you on this? Are there going to be human trials on this soon?
ANTHONY FAUCI: I believe so. I mean, certainly the only human trials that have gone to Phase 3 are the ones that are not going after broadly neutralizing antibodies, that are going after other types of immune responses. But the ones that are going to be going for the broadly neutralizing antibodies are in Phase 1 trial. And hopefully when we get enough information, we’ll proceed to Phase 2a, 2b, and then ultimately to Phase 3.
IRA FLATOW: Compared to 40 years ago our collective worry about HIV/AIDS has largely gone down, of course. But it hasn’t gone away. I mean, I want to cite a 2019 report where more than half of new HIV diagnoses in the US happened in southern states. And of those, African-American men made up a disproportionate number of those cases. How did this dramatic demographic shift happen?
ANTHONY FAUCI: Well it happened, I believe, because of the accessibility of counseling, accessibility to PrEP, accessibility to testing, and ultimately adequate treatment if you prove to be infected or living with HIV. Whereas in some areas of the country, particularly in rural areas of the South which are demographically overrepresented with African-Americans, that the stigma, the lack of access, all of those other factors, have made it very difficult to have that kind of accessibility to all the things that you need to really stop the outbreak, easy testing, lack of stigma, accessibility to care, accessibility to drugs when you need it. There are certain areas of the country where that is not as accessible as in other areas.
IRA FLATOW: I just have a few minutes left. I want to just change gears for a second, because I could not help but ask you something that I just saw released by your office this week. And that is concerning we’re going on with a universal flu vaccine clinical trial, is that correct?
ANTHONY FAUCI: That is correct, Ira. And it’s a viral– it’s a nanoparticle that has on it at least four separate hemagglutinin molecules from various different strains of flu. So what we’re doing now, there’s a number of ways to do that. You can do it by looking, for example, at the invariant part of a single virus. Or you can cluster together on a nanoparticle the hemagglutinin from multiple different ones.
We are very, I would say, cautiously optimistic about this because we feel that this type of technology, this type of platform technology, as new as it is really has a really extraordinary degree of potent immunogenicity of a wide array of responses. So we think that this is hopefully going to be a winner. But we don’t know for sure unless we test it, as you well know.
IRA FLATOW: Yeah. One last simple question for you, how do you feel about your emails getting leaked?
ANTHONY FAUCI: Well, you know, the trouble with that, Ira, is when people look at emails, they then can take anything out of context. They could pull a sentence out without the rest and say that Tony Fauci said this in an email. And it could be a real misconstruing of the real context of what the email is. But the ones that were published in the Washington Post, I mean, there was no problem with that. I think it showed me to be an honest, straightforward person.
IRA FLATOW: Yeah it shows that you’re working very hard.
ANTHONY FAUCI: Yeah, sending emails at 1:30 in the morning.
IRA FLATOW: Yeah, you’re not getting those seven hou– well, you don’t get that many hours’ sleep anyhow, I’m sure.
ANTHONY FAUCI: No, I don’t, Ira.
IRA FLATOW: Well, thank you very much for taking time to be with us today.
ANTHONY FAUCI: I appreciate that. Thank you. It’s good to be with you as always, Ira.
IRA FLATOW: Dr. Anthony Fauci, recipient of the Presidential Medal of Freedom and director of the National Institute of Allergy and Infectious Diseases in Bethesda, Maryland. And hopefully we’ll try this again 10 years from now and see where we stand.
ANTHONY FAUCI: Indeed. Hopefully I’ll be here.
IRA FLATOW: Me too. If you want to go back in time to learn more about the history of the AIDS epidemic in America, including some of my reporting for NPR back in the 80s, you can check out our Science Friday Rewind story at ScienceFriday.com/AIDS. You could revisit all kinds of interviews from the archive and sign up to get future Science Friday Rewind stories. That’s ScienceFriday.com/AIDS.
Copyright © 2021 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Kathleen Davis is a producer and fill-in host at Science Friday, which means she spends her weeks researching, writing, editing, and sometimes talking into a microphone. She’s always eager to talk about freshwater lakes and Coney Island diners.
Lauren J. Young was Science Friday’s digital producer. When she’s not shelving books as a library assistant, she’s adding to her impressive Pez dispenser collection.
Johanna Mayer is a podcast producer and hosted Science Diction from Science Friday. When she’s not working, she’s probably baking a fruit pie. Cherry’s her specialty, but she whips up a mean rhubarb streusel as well.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.