New Drug Reverses Paralysis In Mice With Spinal Cord Injuries
8:09 minutes
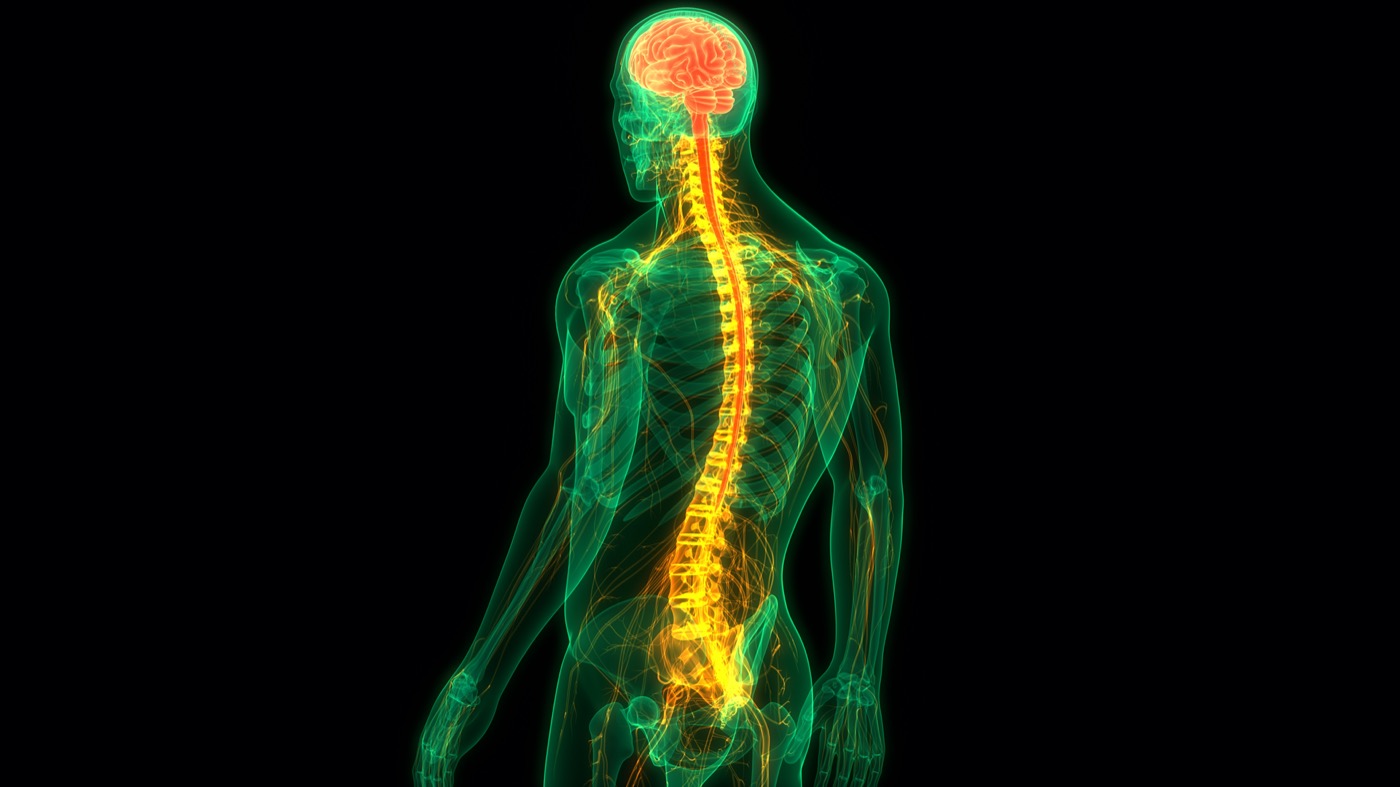
Nearly 300,000 people are living with spinal cord injuries in the United States. Currently, recovery or effective treatment remains elusive. Researchers haven’t yet figured out a reliable way to knit back together severed spinal cords or nerves.
Now, a new study in mice shows promising potential to prevent paralysis after injury. Researchers gave paralyzed mice a specially formulated injection that uses a novel technique called “dancing molecules.” And after a month, the mice were walking again.
Joining Ira to better understand this new development in spinal cord treatment is Samuel Stupp, professor of materials science, chemistry, biomedical engineering and medicine, and director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University in Chicago, Illinois.
Samuel Stupp is a professor of Materials Science, Chemistry, Biomedical Engineering and Medicine and Director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University in Chicago, Illinois.
IRA FLATOW: With nearly 300,000 people living with spinal cord injuries in the US, recovery or effective treatment has been elusive. No one has found a reliable way to knit back together severed spinal cord nerves. But now a study in mice shows promising potential to prevent paralysis after injury.
Researchers gave paralyzed mice a specially formulated injection that uses a novel technique called dancing molecules. And after a month, the mice were walking again. So what are dancing molecules, and how did this all work?
To help us understand what it means for the treatment of spinal cord injuries is Samuel Stupp. He’s a professor of materials science, chemistry, biomedical engineering, and medicine at Northwestern University in Chicago. He’s also the director of the Simpson Querrey Institute for BioNanotechnology. Welcome to Science Friday, Dr. Stupp.
SAMUEL STUPP: Thank you.
IRA FLATOW: How does this injection reverse paralysis in mice? Can you give us some details on that?
SAMUEL STUPP: So the novel therapy is an injection at the site of injury in the spinal cord, composed of invisible, tiny, nano-sized filaments informed by hundreds of thousands of molecules carrying signals to cells in the tissue to initiate regeneration and repair.
IRA FLATOW: And why does your technique work when others have not?
SAMUEL STUPP: Well, there is a key innovation in this therapy. And that is the discovery that when the molecules that carry signals to the cells are undergoing lots of motion within the filaments, they are much more effective at signaling the so-called receptors in cells.
IRA FLATOW: You’ve given a name to this called dancing molecules.
SAMUEL STUPP: Yes. Yes.
IRA FLATOW: Are they really dancing around, like moving?
SAMUEL STUPP: Not exactly dancing, but we thought that was a good metaphor to describe the fact that the molecules within these tiny filaments are walking, translating. They are jumping up and down. And so they are moving a lot.
And the reason this is important is because the signals to initiate repair and regeneration are initiated by the so-called receptors on cell membranes, and the receptors move around a lot. So in a way, the signals have a moving target, if you will. And thus, if the molecules are moving around a lot, they have a much better chance of touching the receptors in the right spot when they are also moving.
IRA FLATOW: Interesting. And so the idea is that someone with a spinal cord injury would get this injection right after the injury, right?
SAMUEL STUPP: That is correct. So in the model that we investigated, the therapy was administered to the mouse 24 hours after the injury. So that means the therapy is designed to treat a new injury to the cord.
IRA FLATOW: Could it treat an older injury too?
SAMUEL STUPP: Well, in principle, yes. It could treat an older injury. And we are, in fact, working on that objective right now. So the therapy itself may be the exact same one. But what has to be different is the way in which it is delivered to the cord. And this will also require some innovation in the surgical technique to administer the therapy.
IRA FLATOW: This is Science Friday from WNYC Studios. Well, that’s really interesting. And I’m wondering, could you apply this therapy– harness it to help treat patients with other types of conditions, like Alzheimer’s or Parkinson’s, or people who’ve had a stroke? Is there a common thread here that would make this new technology useful for a wide range of degenerative diseases?
SAMUEL STUPP: Absolutely. Yes. And this is something that we are very excited about, because we have developed a therapy for the central nervous system, which includes the brain and the spinal cord. And therefore, the types of tissues that we have regenerated and repaired in the spinal cord are very similar to those in the brain. And so we are very interested and excited about considering our therapy for stroke, considering it for brain injuries or for neurodegenerative diseases, and all of those terrible diseases that we’re all terrified of because they impair our cognitive abilities. And so we would like to make a contribution there.
IRA FLATOW: And how soon would we know if this would work in humans? Are there any tests or any planned studies about this?
SAMUEL STUPP: Well, we are going to start, of course, with the spinal cord injury, and specifically with the acute injury, for new injuries, treatment of the new injuries. And we will present our case to the FDA next year. So we are getting ready to go to the FDA in 2022 and present what we have and to ask them what they would like us to do before we can gain approval to test this in human trials.
IRA FLATOW: You know, up to this time, we’ve heard about treatments for spinal cord injury or for other kinds of neurodegenerative diseases using STEM cells. Is there any advantage to your technique over using STEM cells, in experimental form?
SAMUEL STUPP: Well, the advantage of our therapy is in fact that it’s very translatable to the clinic, in principle, because it does not involve the use of cells. I mean, when people think about regeneration, they normally think of STEM cells these days. And cells are difficult to translate as a therapy into the clinic. And there are lots of problems and hurdles to overcome.
It doesn’t involve genes, either, gene therapies, which sometimes can be unsafe. It does not involve the use of proteins and antibodies that might be very unstable or expensive to produce. This therapy is made up of molecules that can be easily manufactured, and therefore has great chance of translation to the clinic.
One other point to make is that the molecules that make up those tiny filaments, the hundreds of thousands of molecules that carry the signals with dancing capacity, I should say– those molecules are made up of the structures of things that we eat every day. So they are made up of amino acids and lipids, so things that are in our foods. And therefore, within a few weeks after the therapy is delivered, the tiny filaments basically biodegrade into nutrients that in turn feed the cells that are in the cord.
IRA FLATOW: Does this mean it might be affordable for patients? Because some of these treatments are really pricey and out of the reach for patients.
SAMUEL STUPP: Yes. Because of all of those reasons I just gave you, I think this will be an extremely affordable therapy, especially compared to the cost of other treatments that are necessary after severe trauma.
IRA FLATOW: Well, Dr. Stupp, we wish you great luck and great success. I think a lot of our listeners will be interested in following your research.
SAMUEL STUPP: Thank you very much.
IRA FLATOW: Dr. Samuel Stupp, professor of materials science, chemistry, biomedical engineering, and medicine at Northwestern University in Chicago. He’s also the director of the Simpson Querrey Institute for BioNanotechnology.
Copyright © 2021 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Shoshannah Buxbaum is a producer for Science Friday. She’s particularly drawn to stories about health, psychology, and the environment. She’s a proud New Jersey native and will happily share her opinions on why the state is deserving of a little more love.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.