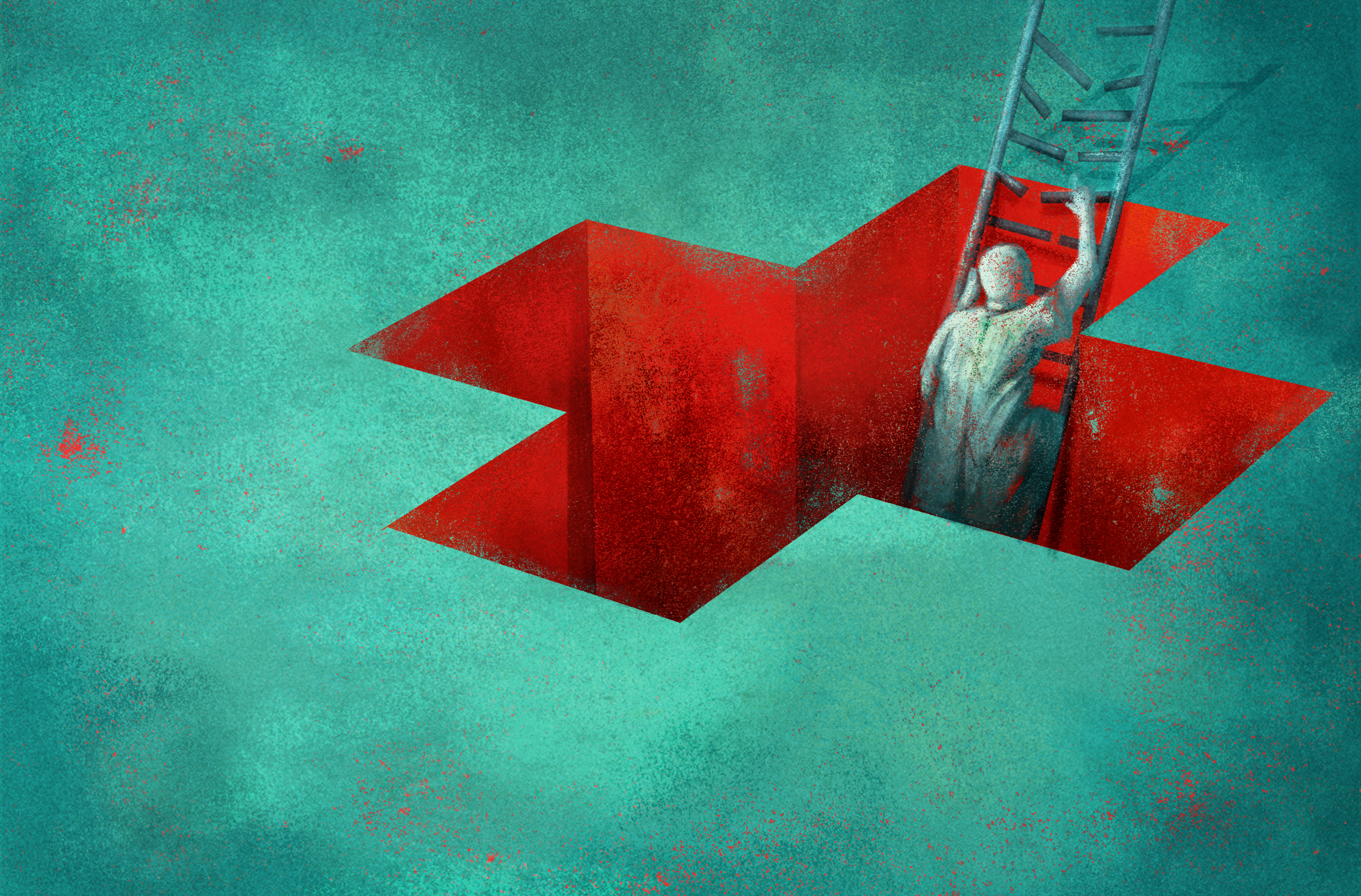
Low Income Patients Hit Hardest By Cancer Treatment Costs
9:32 minutes
Being told you have cancer is not only terrifying, it’s expensive. In the year following a diagnosis, the average cost of cancer treatment is about $42,000, according to the National Cancer Institute.
Some of the newer cutting-edge treatments may cost $1 million or more. While insurance may cover some or all of that cost, many people are uninsured or under-insured. And the bills add up. A quarter of patients with medical debt have declared bankruptcy or lost their home, according to an analysis conducted by KHN and NPR.
While there’s been remarkable progress in treating cancers in the past several decades, less attention has been paid to just how astronomical the price tags can be.
Researchers at Augusta University wanted to track the results of the financial burden after patients’ treatment was complete. They found that poorer patients were hit harder financially—which not only resulted in more bills, but also worse health outcomes.
Ira talks with Dr. Jorge Cortes, co-author of this study and director of the Georgia Cancer Center at Augusta University, about the importance of making cost part of the discussion in developing new cancer therapies.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Jorge Cortes is Director of the Georgia Cancer Center at Augusta University in Augusta, Georgia.
IRA FLATOW: This is Science Friday. I’m Ira Flatow. Getting a cancer diagnosis is not only terrifying, it’s expensive. In the year after diagnosis, the average cost of cancer treatment is about $42,000 according to the National Cancer Institute. But some of the newer cutting-edge treatments could cost $1,000,000 or more. And while insurance may cover some of that, many people are uninsured or underinsured, and the bills add up. A quarter of cancer patients with medical debt have declared bankruptcy or lost their home.
No doubt there’s been remarkable progress in treating cancers in the past several decades, but less attention has been paid to just how astronomical the price tag is. So researchers wanted to track the financial burden of cancer treatments on patients. And they found that poorer patients were hit harder financially, which not only resulted in more bills, but also worse health outcomes.
Joining me to talk about this research is my guest, Dr. Jorge Cortes, Director of the Georgia Cancer Center at Augusta University based in Augusta, Georgia. Welcome to Science Friday.
JORGE CORTES: Thank you very much for having me.
IRA FLATOW: Let’s talk about this study. I know you looked at leukemia and lymphoma survivors across the US, and you found that lower income patients were nearly twice as likely to report poor health outcomes, just about 60% of low income patients. How does this financial burden translate into worse health?
JORGE CORTES: The main focus here is cancer survivors. So we’re talking about patients that already went through all this process of their cancer therapy. And what we found is that there is a significant number of patients who are in the lower income category, and these patients definitely have worse overall health, both physical and mental health after being able to defeat cancer.
So it maintains that lingering effect of the other health issues, as you can imagine. Once you survive cancer, you could have heart conditions, diabetes, or other health problems that you also need to take care of. Some of them may be that you had them already, some of them may be consequences of the cancer or the treatment itself.
And one important thing is that these patients, there is an excess of these lower income patients in the younger population. So these are patients who could potentially contribute to society, who have families, who have a long life ahead of them, and yet they have more issues being able to deal with their other health problems.
IRA FLATOW: Were you surprised by this? I mean, why would you expect treatment of lower income patients, vis a vis cancer, to be different than how these other illnesses affect lower income patients?
JORGE CORTES: I think what happens is that some of these patients, if you are lower income, you can go through your cancer therapy because there are some emergency support systems. You can get them into an assistance program for one of these expensive medications. You can provide them housing during the course of the therapy. You can provide them transportation. You can provide them vouchers. There’s food vouchers. There are many organizations that support that. And that’s very good because it allows them to go through the cancer therapy even when they do not have insurance, when they don’t have the means, et cetera.
The problem is that once they finish their therapy, all of that stops, and then they go back to be on their own. And yet they remain uninsured, they remain with lower incomes, and they have much less of an ability to take care of all the other medical problems, which, again, may be amplified if there are some residual issues related to the cancer or the cancer therapy.
IRA FLATOW: So what can you do? I mean, what do you do then about post-treatment for cancer and having your patients have a better quality of life?
JORGE CORTES: Of course, an obvious answer is, well, we need health care for everybody. But that’s a difficult topic, and it’s obviously something that we need to aim for, but it’s not as easy to implement. But I think there are other elements that we can start being more proactive in doing.
One of them is there is more and more emphasis on starting considering the survivorship of a patient at the time of their diagnosis, not at the time that they finish their therapy for cancer, because that allows you to identify the social circumstances, the financial problems that the patient may have, their family situation, their work situation, et cetera, and try to assess how are you going to navigate through that during the course of therapy and after the course of therapy.
The other thing is there is an increasing use of what we call financial navigators who go through all these financial issues with the patient, and, again trying to use that support not only for their current needs, but also what they will need later on so that they are better prepared. Now that’s certainly not enough. If they’re uninsured, there’s sometimes not too many options. But you can help them investigate the potential support elements that they might find.
IRA FLATOW: And that’s my next question. Where do these people, where do poor people who may not have access to transportation or other resources, how do they find the help they need, the kind that you’re talking about?
JORGE CORTES: Well, and that’s an important element. For the cancer itself, the distance from where you live to a Cancer Center has a negative impact. The farther away you live from a Cancer Center, the less likely you are to survive. We’ve investigated that, and it is very clear.
And it’s not just a matter of providing transportation because you can give them a means of transportation, but they still cannot leave their families behind, they cannot leave work, and so on. So it’s a complex issue.
For their primary care needs, the important thing here is to communicate very closely with those physicians and their oncologists so that they integrate the therapy, and they only come to see the oncologist when it’s absolutely necessary, but take care of their needs locally when that is appropriate. Integrating those, the care of the specialist and the primary care, is critical to provide the best care for their patients closer to where they are.
IRA FLATOW: Have you been able to implement these ideas at the Georgia Cancer Center where you work?
JORGE CORTES: We are certainly implementing the financial navigators much more proactively at the beginning, and we are starting to do these survivorship plans at the time of diagnosis. But there’s a lot of work that we have to do.
I think that telemedicine is something that we did well during COVID, but I think that we need to take advantage of that a whole lot more so that we can continue supporting our patients from a distance. But unquestionably, we need to do more.
IRA FLATOW: And what can you do about the exorbitant cost of cancer treatments? I know you’ve been pushing for more conversations about these for years. Why haven’t cancer researchers been more focused on this?
JORGE CORTES: I think that the problem with the cancer therapies is that there’s no question that developing a new drug is very expensive, but I think that we need to start looking at better models that keep a balance of being able to make these very remarkable advances that we still need, no question, but where there is more of a balance of the value of the benefit that they bring.
Some of the new agents that come end up being very costly, and the return is very modest, possibility of living for a month or two longer, which statistically may sound great. But realistically, especially if the cost is exorbitant, talking about a month or two and you leave a family in financial ruin. So I think there has to be more of an analysis of the value and more of critical view about where are the biggest needs.
IRA FLATOW: Do you sense any shift in the conversation among your peers, among cancer researchers thinking more about cost and access when developing new treatments?
JORGE CORTES: Yes. Fortunately, there is more conversation. I think there has to be more action as well. But definitely, this is something that’s, even on the scientific papers that used to focus only on high end research in the laboratory and these very complex clinical trials, you’re starting to see more and more discussion and studies about the impact of the financial consequences of the drug, of the care, and things like that. Not enough, undoubtedly, but at least it’s taking more of a frontline discussion rather than just being there as a, well, you know, what can we do.
IRA FLATOW: Dr. Cortes, I’m glad we could have this discussion today.
JORGE CORTES: I really enjoyed it, and thank you very much for having me.
IRA FLATOW: Dr. Jorge Cortes, Director of the Georgia Cancer Center at Augusta University based in Augusta, Georgia.
Copyright © 2023 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/.
Shoshannah Buxbaum is a producer for Science Friday. She’s particularly drawn to stories about health, psychology, and the environment. She’s a proud New Jersey native and will happily share her opinions on why the state is deserving of a little more love.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.