Brain ‘Organoids’: Lab-Grown Cell Clusters Model Brain Functions
13:20 minutes
Brain organoids are grown in a lab using stem cells, and can mimic the functions of different regions of the brain like the cortex, retina, and cerebellum. Though it may sound a bit like science fiction, this technology is increasingly being used to better understand brain disorders and eventually develop better treatments.
Ira talks with neuroscientist Dr. Giorgia Quadrato, assistant professor of stem cell biology and regenerative medicine at the University of Southern California, about the state of brain organoid research and her model that mimics the cerebellum.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Giorgia Quadrato is an assistant professor of Stem Cell Biology & Regenerative Medicine at the University of Southern California in Los Angeles, California.
IRA FLATOW: This is Science Friday. I’m Ira Flatow. For the rest of the hour, we’ll be exploring some of the latest advances in neuroscience. There’s this one thing in particular that seems like, well, science fictiony. It’s called brain organoids. These are clusters of human brain cells grown in the lab, and more and more they are being used to better understand brain disorders and eventually develop better treatments.
Earlier this week, I spoke with a neuroscientist who created a new brain organoid model which mimics the cerebellum. Dr. Giorgia Quadrato is an assistant professor of stem cell biology and regenerative medicine at the University of Southern California based in Los Angeles. Welcome to Science Friday.
GIORGIA QUADRATO: Thank you. Thank you. It’s a pleasure to be here.
IRA FLATOW: It’s so nice to have you because you’re working on something really exciting, which I want to get right into. What exactly is an organoid, and how do you grow brain organoids in the lab?
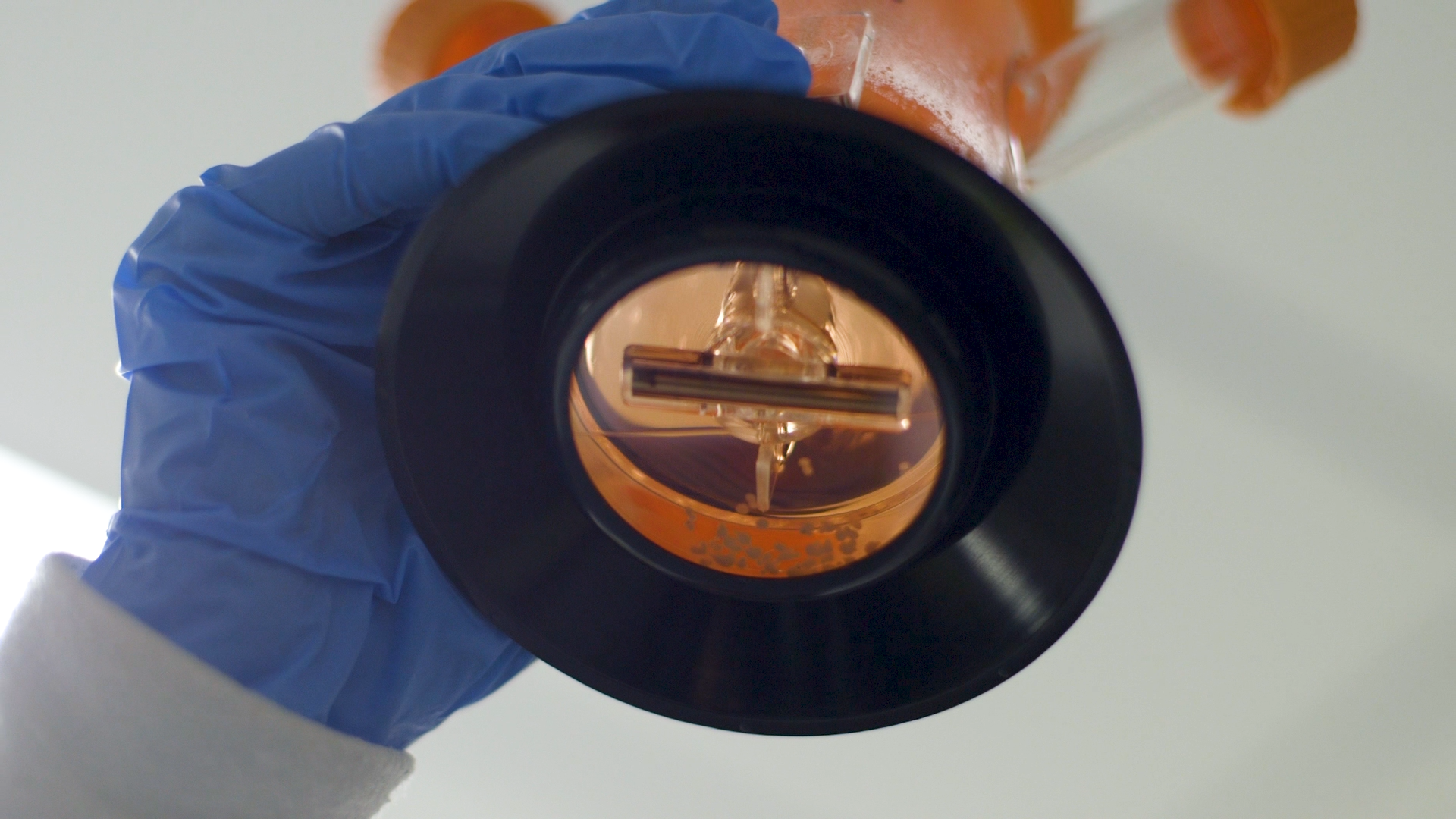
GIORGIA QUADRATO: Yes. Simply put, a brain organoid is a miniature replica of the human brain, and to grow this brain organoid, we start from human pluripotent stem cells. And these are cells that have the capability to differentiate into any cell type of our body. So we start with those. We make aggregate– small aggregates of these pluripotent stem cells, and then we use some chemical factor to differentiate them into different brain tissue.
So the size of these organoids is about 2 millimeters, so they are really, really tiny.
IRA FLATOW: Is that like a grain of rice or something like that?
GIORGIA QUADRATO: Yeah, it’s like– I would say like a lentil. So typically we can culture them up to one year. Over time, they don’t only survive in culture in our laboratory. They actually keep on changing much like our brain does, so they keep on developing new cell type, new type of neurons.
IRA FLATOW: So you can coax these stem cells into becoming one kind of– a certain kind of brain cell, and you’re talking about the cerebellum, correct?
GIORGIA QUADRATO: Yes. Yes.
IRA FLATOW: Why? Why are you so interested in that?
GIORGIA QUADRATO: Actually most brain organoids have been generated to model the cerebral cortex, but my lab is particularly interested in generating cerebellar organoids because the cerebellum is a very fascinating structure of the brain. So first of all, not many people know that about 80% of our neurons of our brain are actually localized in the cerebellum, so it’s a real powerhouse.
IRA FLATOW: Wow. I would have not known that.
GIORGIA QUADRATO: Yeah. It’s a very high computing power because 80% of neurons are there, classically has been always defined as responsible for the execution of locomotion or for keeping balance but actually in the last few years has become more and more evident that the cerebellum is very important also for controlling, for example, emotional responses and behavior, reward behavior, so in general cognitive function. And also something that is very interesting about the cerebellum is that during evolution has change a lot.
So, for example, if we compare the cerebellum of animals in the great ape clade with the cerebellum of a human, they are quite different. And so this is, I think, very interesting, especially if we compare the cerebellum with other brain structure because other brain structure didn’t really change so much throughout evolution. Instead, the cerebellum did, and so this really speaks for the ability of the cerebellum perhaps to be responsible for some of the function that really makes us human.
And so this is why we are very much interested. We believe that problems in the cerebellum can actually also lead to neuropsychiatric disease, which is something that is very much of interest for my laboratory. So we are really much interested in modeling neuropsychiatric disorders.
IRA FLATOW: And are you cultivating a certain kind of cerebellum cell?
GIORGIA QUADRATO: Actually, so what I think is exciting about this new research from my laboratory is that we have been able to generate a cerebellar organoids that contain all the main cell types that we have in the human cerebellum. So they are really all there. In particular, we are very much excited that we’ve been able to generate some progenitor cells that have been recently associated with the pathogenesis of medulloblastoma that is one of the most common pediatric cancers.
And also I think the most important relevant innovation in our organoids is that we have been able to generate Purkinje neurons. So these are specific neurons of the cerebellum that are among the largest neurons in our brain, and these neurons are affected by different types of issues. For example, they can be affected by toxic exposure. For example, alcohol or lithium can damage Purkinje neurons. They are also damaged in some genetic condition, for example, for cerebellar ataxia and also in individuals with intellectual disabilities or autism spectrum disorders. we see problems and degeneration of these Purkinje neurons.
IRA FLATOW: And so you think maybe you can by understanding the cerebellum and the Purkinje neurons better perhaps find treatments for those kinds of illnesses?
GIORGIA QUADRATO: Yeah, exactly. So this is really our final goal is really to– now that we are able to generate Purkinje neurons in vitro so we can really use them to screen for new therapies so first of all, understand better this disease and then trying to find new therapeutics. Basically, before we published this work, previous research was able to generate Purkinje cells but only co-culturing them with mouse cells, other type of mouse neural cells.
The beauty about of our system is that they are developing an all human system. And so all the cell types in these cerebellar organoids are human, and this is important for screening therapeutics that then can be used in human beings.
IRA FLATOW: That’s interesting. And because you have human cells, you can get a much better comparison than you would let’s say using mouse brain cells here?
GIORGIA QUADRATO: Yeah. So I think obviously using mouse models is very important to understand disease and these are in vivo models so they have their advantages, but I think what’s the beauty about this human cerebellar organoids and human cell-based assays in general is that we really can replicate the human genetic background.
So, for example, for neuropsychiatric disorders, the genetic of the person that is affected by the disorder is very important. If the same mutation in the same gene can really lead to completely different clinical manifestation in two different individuals. Because– and this is due to the fact that different individuals have different genetic background. So it is very important to develop models in which we can replicate the genetic background that then leads to basically the clinical manifestation and so the development of some of these neuropsychiatric disorders.
IRA FLATOW: Is the idea that you might take individual cells from people and use their own stem cells so that the genetics is very close to that person and then craft an organoid, is this personalized medicine or not, or is this just basic research?
GIORGIA QUADRATO: This is really– I think one of the most important point that you brought up, our ability with these human-induced pluripotent stem cells to really do personalized medicine. So, yes, we basically we can if we have a patient, for example, with a certain disorder that we want to study, we can take somatic cells from this patient, which means, for example, skin cells or blood cells and then revert them to pluripotency so we can make stem cells, pluripotent stem cells, out of these, and then these cells will actually retain the genetic background of the person obviously. And so we can make mini replica of the brain of that specific person.
And so we are able to then understand the disease of that person very well, and ideally what we would like to do to understand what went wrong in the development of the brain of specific person is to go back in time and look at how that brain develop in the womb. Obviously we cannot do that, but what we can do is grow a brain organoid and see how it develops. So, yeah, exactly so. This is personalized medicine.
IRA FLATOW: OK, so everybody who hears this right is going to want to know how do I take advantage of that. When will it be available for me or my loved ones who may be suffering from some kind of illness? It’s going to be– we’re years away, right?
GIORGIA QUADRATO: Yeah. I think we are years away and there are all these issues also ethic issues related to informed consent, how we deal with this information that we generate from things related to privacy, And so there is a lot that we need to work out for these and also, it’s a matter of cost.
IRA FLATOW: Ahh, cost. Yeah. We’ve never heard that before.
[CHUCKLING]
You love working on the cerebellum, and that’s what your lab is working on, creating organoids which mimic that part of the brain. Now they’ve got to be other people working on different parts of the brain, right, to make organoids for those. Here I’m thinking is it possible to link all of them together so they can all work similar to how our actually whole brain works.
GIORGIA QUADRATO: Yeah. So this is a really fantastic question. Actually in my lab, we also work with other brain organoids from other brain regions, and we are already thinking along this line. There are some other laboratories that have been fusing organoid from different brain regions to study communication between different brain regions. We think that there is a lot of improvement that we can actually– we need to work on this so that we can– so the goal for us is to connect these brain organoids in a way that resemble connection in the actual brain. And again I think to be able to achieve this, we need to bring in people with the expertise in tissue engineering which is what we are doing.
There is really a big opportunity in really connecting organoids from different brain regions because, for example, if there are some diseases that affect only specific brain regions, but we are unable sometimes to discriminate and to understand which brain region is actually causing the disease because brain regions communicate with each other. And so ultimately, when we look at an MRI or some functional imaging, we see that there is a problem in multiple brain regions, but we cannot understand from which one the problem is stemming.
Organoids really give us the opportunity to mix and match brain organoids from, for example, healthy individuals that do not have the disease, so we could use, for example, an organoid that is healthy and then link it to an organoid that is diseased and so and then do the contrary and basically try to understand which brain region is basically important for causing the disorders. So I think this is very important.
IRA FLATOW: Wow. How exciting is this for you to be able to do this?
GIORGIA QUADRATO: Yeah, it’s really super exciting. I mean, I really think– if we think about neuropsychiatric disorders that as I said are really very complex from a genetic point of view, in the last like 70 years, we really haven’t been able to come up with effective treatments for these disorders. And as I said, I think one of the main reason is the incredible complexity of the genetics of these disorders. So I think now with these organoids, we really have the opportunity to understand a lot more about this disease, and so I’m very excited.
IRA FLATOW: This is fascinating, Dr. Quadrato. This was just terrific. Thank you for taking time to be with us today.
GIORGIA QUADRATO: Yeah, my pleasure. Thank you so much.
IRA FLATOW: Dr. Giorgia Quadrato, assistant professor of stem cell biology and regenerative medicine at the University of Southern California in Los Angeles.
Copyright © 2023 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Shoshannah Buxbaum is a producer for Science Friday. She’s particularly drawn to stories about health, psychology, and the environment. She’s a proud New Jersey native and will happily share her opinions on why the state is deserving of a little more love.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.