How AI Could Predict Heart Disease From Chest X-Rays
7:38 minutes
Research on medical uses for artificial intelligence in medicine is exploding, with scientists exploring methods like using the retina to predict disease onset. That’s one example of a growing body of research on “opportunistic” AI, the practice of analyzing medical scans in unconventional ways and for unintended diagnostic purposes.
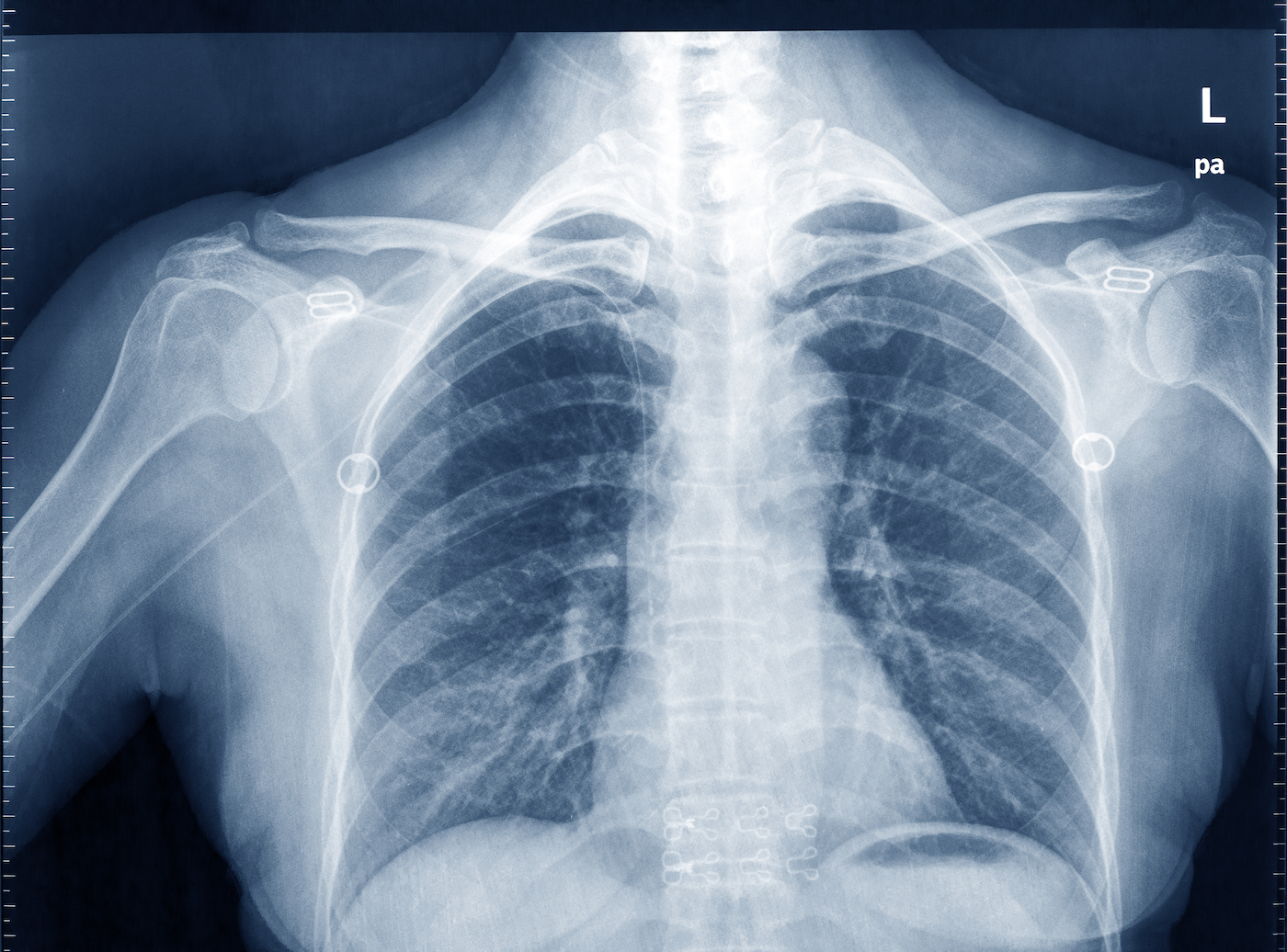
Now, there’s some evidence to suggest that AI can mine data from chest x-rays to assess the risk of cardiovascular disease and detect diabetes.
Ira talks with Dr. Eric Topol, founder and director of the Scripps Research Translational Institute and professor of molecular medicine.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Eric Topol is a genomics professor at the Scripps Research Institute in La Jolla, California, and the author of several books.
IRA FLATOW: This is Science Friday. I’m Ira Flatow.
The last time Dr. Eric Topol came on the show, he talked about the exciting new ways that artificial intelligence might help physicians make better diagnoses, like using the retina to predict disease onset. Well, now there’s some new evidence to suggest that AI can mine data from chest X-rays, too, so he’s back to fill us in on this.
Dr. Eric Topol, founder and director of the Scripps Research Translational Institute, professor of molecular medicine, based in La Jolla, California. Welcome back to Science Friday. Always great to have you.
DR. ERIC TOPOL: Thanks so much, Ira.
IRA FLATOW: In your newsletter this week, you wrote about a study that showed that AI could better gauge a patient’s risk for heart disease by looking at a chest X-ray, as compared to standard ways doctors gauge risk. How do cardiologists typically assess heart risk for patients, and how might this be different?
DR. ERIC TOPOL: Yeah, this one is really wild, Ira. There’s been several of these so-called opportunistic studies, where you get information from a scan that we would never have envisioned as possible. The normal way we look at it is there’s nine variables that include blood pressure and cholesterol and several others, and that predicts a person’s 10-year risk of having a heart attack, a stroke, or cardiovascular death.
So that’s based on Framingham and many other studies, and that’s what’s been used all these years. Who would have ever thought that you could get better information from the chest X-ray?
IRA FLATOW: Well, tell us about that? What kinds of information does AI pull out of it that’s so useful?
DR. ERIC TOPOL: I wish we knew. [LAUGHS] This is the problem. Some of these opportunistic studies have really delved into explainability.
Like, for example, another chest X-ray study that diagnosed diabetes– which, again, I would never have thought that was possible, right– from the chest X-ray. It basically did this so-called occlusion, or masking, where it would look at the chest X-ray and block out various regions to find out what was the source of the information that we can’t see. And it turned out it picked up the fat pads in the chest that was providing this diabetes possible diagnosis.
But for the risk of heart attacks and stroke, we don’t know how it was so powerful and better than our standard. So this is part of that X factor that we still need to learn.
IRA FLATOW: Well, I’m still not quite understanding this. I mean, how did the AI– what did it see in the chest X-ray that told doctors– or it found that the patient’s risk for heart disease was greater?
DR. ERIC TOPOL: Well, we can tell from other studies using the chest X-ray for this opportunistic detection that it can pick up the calcium score– what people can undergo a CT scan to see how much calcium they have in their coronary arteries. But that can be derived from a chest X-ray, and that is an indicator of risk.
Also, the chest X-ray can be– through AI, determine the heart strength– the so-called ejection fraction. So it’s picking up a bunch of things, as seen in other studies, that are very predictive of a person’s risk. And it must be the composite of these things.
But we really don’t know because, although the study really was extraordinary, it didn’t do enough as far as the explainability side of things. So that’s where some of the work that needs to be done– and it needs to be replicated before this becomes a standard way to predict risk of a person’s heart or stroke in the ten years ahead.
IRA FLATOW: And one of the things you point out in your newsletter is that there are so many chest X-rays done each year, right? And you could repurpose them without having to take an additional one.
DR. ERIC TOPOL: Exactly. The fact that there are over 70 million chest X-rays in the United States each year alone– it’s incredible. So there’s all this free added information in those chest X-rays that could help us because most people don’t know their cardiovascular risk. And that’s important, especially for determining whether a person should take a statin, and whether it should be an intensive statin type of medication and dosage.
So there’s lots of things that can be done to mitigate risk. It isn’t just that you’re going to have this bad future forecast. There are things that can be done to change it.
So, yeah, as you point out Ira, there’s just so much chest X-ray data out there that isn’t being used today.
IRA FLATOW: And what about– you talked about the retina last time. Now you’re talking about chest X-rays and lungs. What about picking up some other organ? Could we scan some other organ and find other stuff from it?
DR. ERIC TOPOL: Well, another example from the chest CT is the ability to pick up pancreatic cancer because radiologists don’t look at the pancreas in a chest CT. So cancer risk that’s already being done for a scan otherwise.
But the other thing that’s been noteworthy– you mentioned the retina. The electrocardiogram has lots of information. And give credit to the Mayo Clinic– they are the first to now use that opportunistic electrocardiogram to tell all their doctors whether the patient has a low ejection fraction– that is diminished heart strength– and other diagnoses that are not done anywhere else in this country. So we’re starting to see that transition of this being able to detect more and providing that to the patients through their doctors.
IRA FLATOW: Yeah because now that you say that, that stimulates me to think about– could we be picking up something erroneously by using AI that may not be important, but AI thinks it is?
DR. ERIC TOPOL: That’s a really important point. It’s just like when you do scans for a person that doesn’t have symptoms, and you pick up these incidental findings. That could be the problem too– the false positives. So that’s why before these are put into clinical practice on a routine basis, we’ve got to know whether you’re going to get false signals. And so far the data look encouraging, but it’s still early.
IRA FLATOW: Well, if you say it’s still early, and that’s a good point– how do we make it not so early? I mean, what needs to be done?
DR. ERIC TOPOL: Well, ideally, we’d have at least one more study to confirm the new one for the chest X-ray and picking up the risk of a person. And we’d have a much better handle on how did it do this? How did the AI figure out this risk so precisely? Better than all of the studies that have been done for the last many decades, right? So we just got to confirm this and understand it better. But if it really holds, then someday, Ira, this will become a routine output– a readout from chest X-rays.
IRA FLATOW: Well, we’ll wait for that day, Eric. Thank you for taking time to be with us, and come on back when you’ve done some more snooping around.
DR. ERIC TOPOL: OK, will do. Thank you.
IRA FLATOW: You’re welcome. Dr. Eric Topol, founder and director of the Scripps Research Translational Institute, professor of molecular medicine, that’s in La Jolla California.
Copyright © 2024 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Shoshannah Buxbaum is a producer for Science Friday. She’s particularly drawn to stories about health, psychology, and the environment. She’s a proud New Jersey native and will happily share her opinions on why the state is deserving of a little more love.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.