A Dangerous Fungal Superbug In Hospitals Worldwide
17:34 minutes
 Science Friday reported a new multimedia feature on the fungal disease, Valley Fever, which plagues the American West and shows signs of spreading. Read and watch the story on Methods, from Science Friday.
Science Friday reported a new multimedia feature on the fungal disease, Valley Fever, which plagues the American West and shows signs of spreading. Read and watch the story on Methods, from Science Friday.
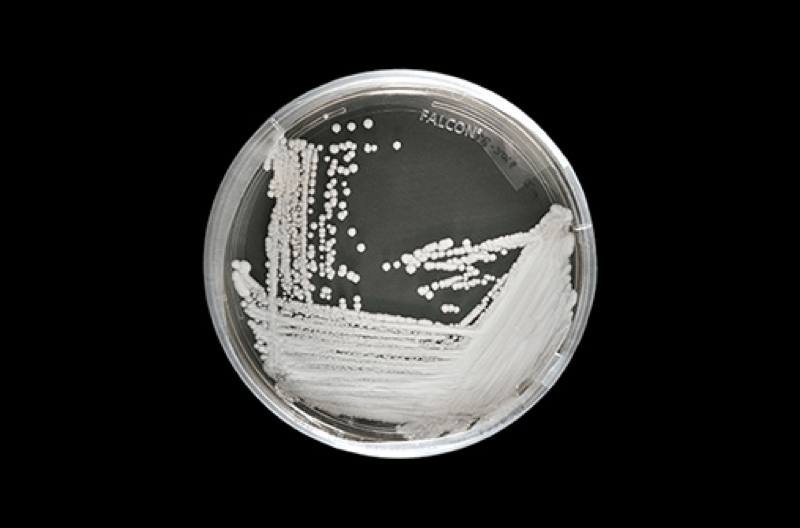
If you hear the word “superbug,” you’re likely to think about drug-resistant bacteria or even viruses. But in a case that’s been unfolding since 2009, a drug-resistant yeast is increasingly worrying epidemiologists. The yeast, Candida auris, has popped up in 27 countries so far, with 340 cases in the United States. It has a mortality rate of 60 percent.
Unlike other kinds of fungal infection, C. auris seems able to hop from person to person and persists on sterile surfaces. Inconveniently, the yeast’s spores are unusually resilient against standard hospital cleaning solutions. On top of that, it’s already resistant to most of the antifungal drugs in existence—there weren’t many of those to being with.
[Peep the world’s oldest recorded origin of the zero symbol we use today.]
But even before the emergence of C. auris, yeast and other fungi were already a deadly reality for some. You don’t want to come down with valley fever, a potentially deadly fungal lung infection, for example. And other yeasts in the Candida family are a common culprit in hospital-acquired blood infections.
Science writer Maryn McKenna, who wrote about the rise of Candida auris for Wired, joins Ira and CDC Chief of Mycotic Diseases Tom Chiller to discuss the underestimated risks of fungi and how health systems can combat them.
Maryn McKenna is a science writer and columnist for Wired. She’s also the author of Big Chicken: The Incredible Story of How Antibiotics Created Modern Agriculture and Changed the Way the World Eats.
Tom Chiller is the chief of the Mycotic Diseases Branch at the Centers for Disease Control. He’s based in Atlanta, Georgia.
IRA FLATOW: This is Science Friday. I’m Ira Flatow. If you work in a hospital, the last thing you want to deal with are superbugs, usually drug-resistant bacteria– think MRSA– that take advantage of sick and weak patients. But have you ever heard of a superbug yeast?
Perhaps you’ve had a mild yeast infection. Many of us have, but yeast can be fatal in humans. Candida albicans is a major culprit of blood infections that can lead to septic shock, and other fungi around the world can cause lung infections and gastrointestinal problems. But now there’s a new infectious yeast in town that seems capable of spreading as fast as bacteria, persisting outside the human body for long periods of time, and with high mortality in the patients that acquire it. Oh, and by the way, we don’t have a lot of drugs for combating this virus.
Here to tell the tale is Maryn McKenna, she’s senior fellow at the Schuster Institute for investigative journalism at Brandeis University and science writer and columnist for Wired. And she recently wrote about the rise of Candida auris and troubles it could pose for public health. Welcome to Science Friday.
MARYN MCKENNA: Thanks for having me.
IRA FLATOW: Dr. Tom Chiller, chief of my mycotic diseases at the Centers for Disease Control. He joins us by Skype. Welcome, Tom.
TOM CHILLER: Great to be with you, Ira.
IRA FLATOW: Maryn, what the heck is this yeast? Tell us about it.
MARYN MCKENNA: So this yeast only came on the radar of scientists in 2009, initially just via ear infection in an elderly woman in Japan. And that was not that unusual. And then as people started to look at it, they realized that it really was very unusual because this yeast behaves like a bacterium. In fact, everything that we think about that’s bad about superbugs, which are bacteria, is worse in this yeast. There are fewer drugs, it has higher mortality, it spreads in a mysterious manner, it seems to have arisen all over the world at the same time. It’s like superbugs on steroids in a species where superbugs shouldn’t occur at all.
IRA FLATOW: Is it infectious differently? Does it spread differently than other yeast we’re familiar with?
MARYN MCKENNA: So the interesting thing about this is that when you talked in your intro about people being familiar with yeast infections. And most of the time when you have a yeast infection, it’s because you’ve actually inoculated yourself or infected yourself with the yeast that you were already carrying. What’s different and troubling about this new superbug yeast, Candida auris, is that it passes from person to person. So it may have originated in one person, but it causes outbreaks through person to person transmission and through transmission by surviving on cold, inorganic surfaces. That’s totally new.
IRA FLATOW: Do we have any sense about how many people may have died from this new yeast?
MARYN MCKENNA: So there have been 340 cases, I believe, in the United States, but I’m sure that Dr. Chiller’s more up on the numbers than I am.
IRA FLATOW: All right, Dr. Chiller, can you fill us in on that?
TOM CHILLER: Sure, I’d be happy to. And just back to Maryn’s point about these organisms generally being with us. So we think of the organisms that are in our intestines as part of our, what we call, normal flora. We have trillions of bacteria there. We also have trillions of Candida. So Candida has been with us, evolving, for millions of years and it’s interesting to note that this particular Candida, as Maryn described, isn’t in that space. They’re not thought to be part of our normal flora, as we like to call it. But instead they’re on our skin, and they seem to be very happy on skin and other surfaces. And therefore, transmit much more readily between people or from people to surfaces and then from those surfaces to people.
As far as the numbers of infections and people with this infection that we’re seeing, there’s a wide variety of ways in which we’re finding this. So the most severe and significant, obviously, is when this organism gets into the bloodstream. And so far, in the United States, those patients are very medically experienced. So they’re quite sick, quite ill, are very much exposed to hospital environments. And those are the patients that we’ve seen in the hundreds that have it in their blood. There are many people that have it on their skin that are also in these health care environments, but at least if it’s on the skin It can be contained or one can try to contain it.
In other countries, the situation is a bit worse. And there are some countries where now 40% of the bloodstream infections caused by Candida are actually caused by this Candida auris. And that’s really our concern in public health as we’ve seen where it can spread and become very dominant and that’s one of the things we’re concerned about here.
IRA FLATOW: Our number 844- 724- 8255. You can also tweet us at SciFri. You know, we don’t hear a lot about killer fungi as much. Is this because they’re just not as good at infecting us? You say they’re a natural part, normally, fungi of our microbiome, and so this is sort of an outlier then?
TOM CHILLER: Yeah, I mean, I think there’s a couple of things going on. Number one is fungi generally are opportunists. So they live with us and then if there are some breakdown in our skin barriers, breakdown in our intestines, you have surgery, you have an intravenous line in, they can get in and invade and cause problems in our blood. But there are also lots of fungal infections out there that are just misdiagnosed or underdiagnosed.
We unfortunately, for all the different types of infections that we see, have a real hard time diagnosing fungal infections and we really need to develop more diagnostic tests to diagnose these diseases.
IRA FLATOW: So Maryn, now that we know a little bit more in the news about this and just fungal infections is getting out, how are the hospitals responding to this? What can they do?
MARYN MCKENNA: So this is really a problem. I think when people think about superbugs, they realize that outbreaks within hospitals among the sickest patients. That’s sort of how superbugs surfaced. That’s where we notice them first. That’s where they pose the most challenges. And every superbug over the past 20 years or so has taught us something new about the kind of threat they are.
So MRSA, which you mentioned, came along. It lives on skin and so hospitals had to learn that everyone had to wash their hands really well. Then the CREs, the highly resistant gut bugs, came along and people realized, oh no, things live on surfaces as well, so we have to learn how to clean the hospital environment.
Now Candida auris pushes us further than that because the things that we’re using to clean the hospital environment, which is mostly cleansers based on quaternary ammonium, don’t appear to kill this bug. So we have to go back to much more harsh cleansers that generally aren’t used because they’re kind of destructive to things that exist in hospitals. And also to the kind of old-fashioned, but reliable but not as thought of infection control practices like putting patients together in one part of the hospital, putting patients in isolation, making sure everybody thoroughly gowns and gloves and masks up before seeing them. It requires a lot more attention to really fine details of infection prevention that, with Candida auris, you just can’t slide.
IRA FLATOW: Just going back to the future, is what you’re saying. Health care-wise and cleanliness, washing hands, possibly using more toxic–
MARYN MCKENNA: And it sounds like that ought to be simple, right? But from 25 years of hospitals working on things as simple as washing hands, there have been studies after studies that show that health care personnel actually aren’t all that good at washing their hands, even when they know someone is watching them to see if they do it. So these things that sound very simple, they’re actually hard to do.
IRA FLATOW: Tom, you agree?
TOM CHILLER: Yeah, and I think just to add to what Maryn is saying, these physicians and health care providers, when they think of Candida– as you mentioned at the beginning, Candida albicans, a very common Candida in our intestinal tract, which can cause bloodstream infections– and does. And is, in fact, very common cause of bloodstream infections in hospitals, is not something the health care providing community worries about transmitting.
So as Maryn mentioned, it’s almost as though you infect yourself with the organism that’s in your GI tract, because the barriers have broken down because you’re in a health care facility and you’re getting treatment. So this organism, Candida auris, is not acting that way, and so part of this is just the awareness. We don’t generally react to a Candida species with intense infection control and disinfection. And so part of this is just getting the health care community more aware that for this particular organism– which is a Candida that normally you don’t react to– here, you have to react.
And on top of that, as you probably mentioned at the beginning, to me the definition of a superbug is something that’s highly resistant to the available treatments. Unfortunately, unlike the bacterial world, in the fungal world, we have really three main anti-fungals that we can use for invasive infections. This organism has been found to be resistant to all three in some, thankfully rare, situations. So that leaves us with no options.
And that’s really the other big concern is that if this is able to get a foothold and set up shop, so to speak, and become more globally spread, then we’re going to worry about our ability to be able to treat the serious infections.
IRA FLATOW: We hear all the time, Maryn, that drug companies don’t want to get involved in something if there’s not money to be made because there are not enough people being infected to sell their drugs to. Will that change now if people start hearing about and panicking about–
MARYN MCKENNA: I wonder. I mean, we’ve been panicking about bacterial superbugs and the loss of antibiotics for quite a while now, and yet, most of the companies that once made antibiotics have moved out of that manufacturing space because they say– with actually fairly good data to back them up– that it’s not in their economic best interests to make antibiotics. They just don’t make their R&D money back. So at this point, though Candida auris is highly fatal to people, has really high mortality rates, there aren’t all that many cases. Does that, therefore, mean that companies are going to rush into this space to make these drugs when they haven’t rushed into the space to make drugs for bacterial superbugs? That seems unlikely to me.
IRA FLATOW: Tweet coming in from David Eckard who says, how much of it is airborne? Can it be spread? I think you mentioned by the skin. Dr. Chiller, how much can it be spread through the air?
TOM CHILLER: Yeah, that’s a good question. Honestly, Candida, in general, we don’t think of as an airborne fungus. There are plenty of other fungi. In fact, most fungal infections that do invade do come in through the lung, but in this case, Candida generally does not. Again, it’s in our intestines and it’s on our skin and so it’s transmitted by touch. But there’s still a lot unknown about Candida auris, and so I think we still need to understand whether there is the potential for this to be aerosolized. But it’s certainly not the primary way that it’s spread.
IRA FLATOW: And we’re getting a bunch of tweets saying the same thing– is this something I should be worried about at home or are we only talking about hospitals as the places where this is being spread?
TOM CHILLER: Yeah, I think that’s a really important question because, no. I think that the shorter answer is, this is not something that I want the general public to go home and be concerned about. This is, right now, one of these organisms that is very health care associated, that is really set in health care settings. But both the hospitals and the longer-term care facilities are having issues with this. And it generally, again, affects people that are sick and have been exposed or, as we like to say, medically experienced. But I do think it’s important for the general public to know about it and to know that their loved ones that may be in hospitals could be getting this or could be exposed to this. And so it’s important to know what you’re getting into in a health care environment.
IRA FLATOW: I’m Ira Flatow. This is Science Friday from WNYC Studios. Talking with Tom Chiller and Maryn McKenna about this new superbug fungus among us. I can see from my Twitter board lighting up and whatever, people are saying, uh oh, I’m going home with a bottle of bleach. I’m going to start spraying everything. This is not something they should be doing. Maryn?
MARYN MCKENNA: So, true. People should not be spraying their households with bleach. Bleach is bad for your clothes and bad for your lungs and just not a good–
IRA FLATOW: Someone here says oven cleaner.
MARYN MCKENNA: Even worse. Let’s not do that. Let’s not go sterilize our entire environments. However, I think what Tom said is really important. What’s become clear in the past couple of years in sort of studies of superbugs and infection control is that no hospital is an island. They exist in very complex networks of nursing homes and long-term assisted care facilities and people move in and out and back in kind of unpredictable ways. So to say that it’s only a risk in hospitals, which sounds like, oh, it’s never going to affect any of us, actually means that it’s a risk in hospitals and in all the other institutions that touch hospitals. And we shouldn’t discount it as a public health threat just because it’s not going to show up in our kitchens the way drug-resistant salmonella does.
IRA FLATOW: And Dr. Chiller, picking up on your point before about saying, you know, we need to take fungal infections more seriously now, like we do some of the bacterial infections.
TOM CHILLER: Yeah, I think that we are trying very hard, certainly, in the fungal infection world, to advocate and make people aware that these infections are occurring and they occur actually quite frequently. They’re often misdiagnosed and one of the problems with misdiagnosis of fungal infections is they get treated like bacterial infections. And so we know patients will get courses and courses of antibacterials, which, of course, are then killing off the good bacteria that you have in your GI tract or in your intestines. And then they can actually cause fungal infections to become worse because you’ve now out-competed everything that is competing with the fungi. So there’s a lot to be said about thinking fungus, and we try to have awareness campaigns around think fungus, and this is both for the public and for the health care communities as well.
IRA FLATOW: Is climate change going to affect the spread and toxicity of these fungus?
TOM CHILLER: Well, certainly fungi are environmental organisms. So they live in the environment. Now there are, as we’ve talked about, some Candida are part of our commensal organisms, part of our microbiome, as you mentioned. But most fungi live in the environment, and so changes in the environment change the fungi that are there. They can either proliferate or they can die off. They can be selected for resistance depending on what types of pesticides and other things are used in the environment.
So certainly, environmental changes dramatically affect the fungi. And we know this when we’re looking at a disease that we call valley fever that is caused by a fungus down in the Southwest. We know that drought and rainfall can dramatically affect different infection rates on the years depending on whether there’s been lots of rain followed by drought, et cetera.
IRA FLATOW: And Maryn?
TOM CHILLER: These are other environmental organisms and the environment changes affect them for sure.
MARYN MCKENNA: So one of the intriguing mysteries of Candida auris is, remember, this is a really new species that was only identified 10 years ago. It appeared in four different places around the world at the same time, didn’t spread from one to the other three. What happened to make it appear in all those places at once? That’s one of the questions that has to be answered. And it seems as though the environment ought to have played a role.
IRA FLATOW: All right, that’s a good way to end the program– with a question, which I always like to answer later. Maryn McKenna, science reporter and columnist for Wired. Tom Chiller, chief of the mycotic disease branch at the Centers for Disease Control and Prevention in Atlanta.
Thank you both for taking time to be with us today.
MARYN MCKENNA: Thanks.
TOM CHILLER: Thanks for having us.
IRA FLATOW: We’re going to take a break and when we come back, we’re going to talk about the paleo diet of dinosaurs. How nutritious was the dino dinner and how do we know how much they actually ate to survive? These big dinosaurs, you know, herbivorous ones. We’ll talk about someone who measures that in her lab. Stay with us. We’ll be right back after this break.
Copyright © 2018 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Christie Taylor was a producer for Science Friday. Her days involved diligent research, too many phone calls for an introvert, and asking scientists if they have any audio of that narwhal heartbeat.