Could Vaccines Of The Future Be Made With Nanoparticles?
11:51 minutes
In 2021, vaccines for COVID-19 were released, a little over a year after the SARS-CoV-2 virus triggered a global pandemic. Their remarkably short production time wasn’t the result of a rush-job, but a culmination of decades of advancements in infrastructure, basic science, and mRNA technology.
But despite the years of innovations that allowed those vaccines to be developed and mass-produced so quickly, their delivery method—an injection—still has some drawbacks. Most injected vaccines need to be kept cold, and some require multiple trips to a pharmacy. And people with needle phobias may be reluctant to get them altogether. So what could the vaccines of the future look like?
Dr. Balaji Narasimhan, distinguished professor and director of the Nanovaccine Institute at Iowa State University, joins Ira Flatow onstage in Ames, Iowa, to talk about how his lab is using nanotechnology to develop the next generation of vaccines, and how they could be more effective than current vaccines in the face of the next pandemic.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Balaji Narasimhan is a distinguished professor and the Director of the Nanovaccine Institute at Iowa State University in Ames, Iowa.
IRA FLATOW: This is Science Friday. I’m Ira Flatow live from Iowa State University in Ames.
[APPLAUSE]
In 2021, vaccines for COVID-19 were released just a little over a year after the virus caused a global pandemic. Their remarkable short production time wasn’t the result of a rush job, as you might have heard, but a culmination of decades of advancements in infrastructure, basic science, and mRNA technology.
But despite the years of innovations that allowed those vaccines to be developed and mass produced in just a year, their delivery method, the needle, right? The needle, the dreaded needle, is pretty old technology that has some significant drawbacks. So what could the vaccine, what could it look like?
That’s what we’re going to talk about with my next guest, Dr. Balaji Narasimhan, distinguished professor and director of the Nanovaccine Institute at Iowa State University. Welcome to Science Friday.
BALAJI NARASIMHAN: Thank you.
IRA FLATOW: OK, so vaccines are great. Modern vaccines are great, but they have a few drawbacks. Tell us what you think they are.
BALAJI NARASIMHAN: So first, thank you for having me on the show, Ira. So today’s vaccines are being manufactured with what I would call legacy technologies, technologies that have been around 70, 80, or 100 years. Many of them use chicken eggs and grow viruses in chicken eggs, and that is a technology that’s old, and it takes a long time.
Our vaccines are also made in a way that they’ll only work if they are kept cold.
IRA FLATOW: Really cold, right?
BALAJI NARASIMHAN: Really cold. So I don’t know if you remember this, but you mentioned 2021. So labs like mine were looking for equipping our labs with freezers, and guess what? Walgreens and CVS had all the deep-freeze equipment in the country. So labs like ours had to wait six, seven, eight months before we could get equipment because these vaccines need to be stored cold. And so that is a huge drawback because if you think about transporting these vaccines, if you think about Doctors Without Borders, organizations like that leaving a fridge open for five minutes, you have to throw that entire lot of vaccine away.
IRA FLATOW: Five minutes?
BALAJI NARASIMHAN: Five minutes of exposure to room temperature is enough to destroy the performance of the vaccine. So that is another huge drawback.
As we’ve learned during the evolution of COVID vaccines, these vaccines, the way they’re made today, also need to be updated as we see more and more variants. We started off with the parent version of the virus, and then we all know there’s a huge number of variants that have come down the pike. And the first vaccine that worked is not going to work against the variants of today, so these vaccines also need to be constantly updated. And as you pointed out, Ira, they need to be delivered with a needle, which I think is also a drawback.
IRA FLATOW: OK, yes.
BALAJI NARASIMHAN: I don’t know about you, but I think it’s a drawback.
IRA FLATOW: Well, let’s talk about it because you are working on using nanoparticles that don’t need a needle. Tell us how that works.
BALAJI NARASIMHAN: Right. So the strategy that we use is we want to hit the virus where it resides, right? So if you look at respiratory infections like flu or SARS-CoV-2, which causes COVID-19, or RSV, those pathogens reside in our lungs. So we want to go hit those guys where they reside. So this is like, again, going back to a Star Wars analogy, right? In A New Hope, what was the strategy? Go directly to the source. So that’s what we did. These things hide out in our lungs. So that’s the Death Star for them, and so we need to get our vaccines to where they reside so that they can get rid of those pathogens.
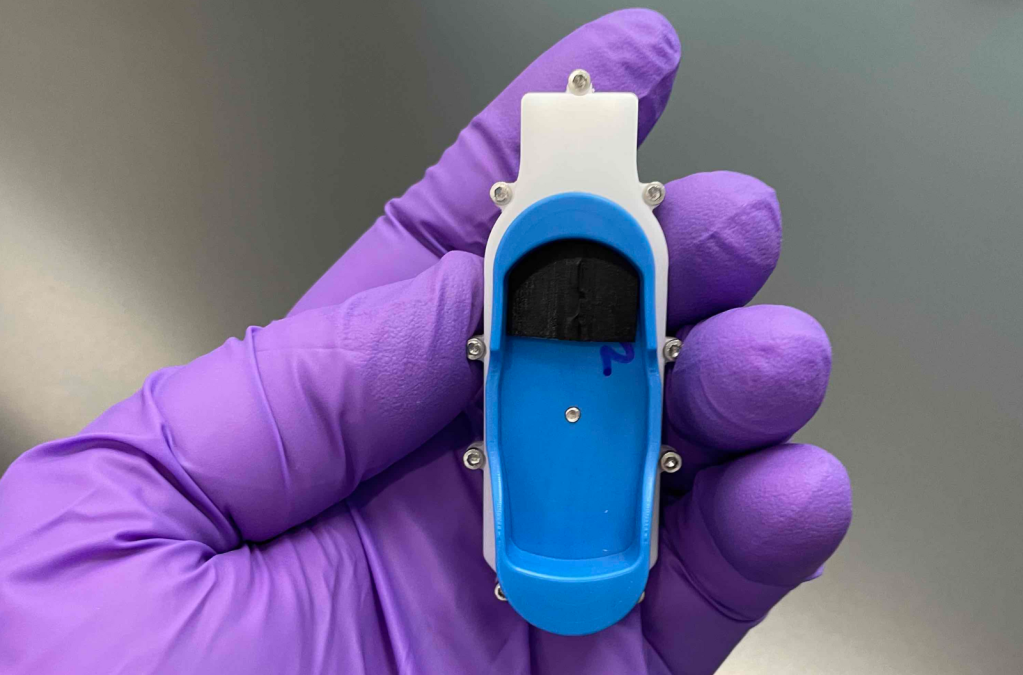
So if you’re looking at respiratory infections, what is the best way to get pathogens or vaccines into the lungs? It is through the use of inhalers. So these nanoparticles that we synthesize in our lab are able to be delivered needle free. So these are vaccines that you can inhale. You can inhale with a very commonly used inhaler-type device, which I have an example of here, which Ira, you can see.
So this is just like any regular inhaler that we’re used to, except that you inhale the vaccine through your nostril. And you can take a sniff of this vaccine, and you’ll have immunity in a week.
IRA FLATOW: A week?
BALAJI NARASIMHAN: You’ll have immunity that will also last for longer.
IRA FLATOW: Why does it last longer?
BALAJI NARASIMHAN: OK, that’s a great question. So these particles that you referenced, Ira, these particles degrade slowly over time. So imagine a bar of soap. So as you keep using that soap, it erodes layer by layer and slowly shrinks in size, right? That’s how these particles are. So they will slowly erode over time, and they will release whatever payloads are inside the vaccines, which are typically proteins, proteins that are specific to the virus that we’re trying to neutralize.
So if you want to design a flu vaccine, you put in flu proteins. If you want to design an RSV vaccine, you put in RSV proteins. So it’s because of their slow degradation that they’re able to release their payload over a long period of time, which gives us immunity that lasts for a long period of time, in contrast to existing vaccines whose immunity wanes over time.
IRA FLATOW: So you don’t need the booster shots?
BALAJI NARASIMHAN: That’s the goal, yes, is that you would need fewer booster shots or, ideally, none.
One of the other properties of this vaccine, Ira, that I’m very excited about that I think is a game changer is that this vaccine is room-temperature stable.
IRA FLATOW: Wow. Wow.
[APPLAUSE]
BALAJI NARASIMHAN: And so if I had this nanovaccine in an inhaler like this and kept it here on May the 4th, Star Wars Day, of 2024 and I came back here to Stephens Auditorium on May the 4th, 2025, 2026, took this inhaler, and used this vaccine, it’ll still work.
IRA FLATOW: Two years later?
BALAJI NARASIMHAN: That’s what our data shows. You can take this vaccine and deliver it to your home. So whenever that future pandemic hits, we want to be ready with technologies like this where the vaccine will be self-administered by yourself. You don’t need a professional to come and give you a shot or two or three. This vaccine could be delivered to your home because it’s room-temperature stable, and you could take a sniff of this vaccine and go back to work.
IRA FLATOW: Wow. Wow.
BALAJI NARASIMHAN: That’s the future. That’s the future that we dream about and that makes us come to work every day morning.
IRA FLATOW: Not only did my mother tell me when something sounds too good to be true not to believe it, but as a science journalist for many decades, I always know there is some drawback to everything. You have to sacrifice something to get something. What’s some of the drawbacks here?
BALAJI NARASIMHAN: So first of all, as I mentioned, even though we manufacture the vaccine with a process that is very well known to the pharmaceutical industry, we manufacture the vaccine using a process called spray drying. We have to demonstrate that we can manufacture at scale, right? This is a country of 300-million-plus people. We need to make vaccines in terms of doses, I’d say, 10, 20, 30 million doses a day. So we have to demonstrate that these vaccines can be manufactured at scale. So that’s number one.
Number two, as I mentioned, today’s vaccines are made using legacy technologies that are 70, 80, 90 years old. Change in industry is a very, very slow ship. So that ship turns very slowly. And so in order to get the pharmaceutical industry, the vaccine industry to buy into these new manufacturing methods so that these vaccines can be made rapidly, especially in response to a pandemic, is the second challenge.
The last one, which I’m actually pretty encouraged to see now, is what we have, Ira, is what I call a platform technology. So it’s a platform technology because it’s plug and play. We were working on a flu vaccine when COVID hit, and we literally got an opportunity to pivot to seeing if our plug and play that we claim works very well would work with our COVID vaccine, and it did.
Whenever that pandemic is going to hit, these platform technologies, which can be packaged in devices like this, is what’s going to help us get vaccines fast and to people where it’s needed.
IRA FLATOW: Let’s go to a question from the audience over here.
AUDIENCE: Thank you. So basically, you told about how these nanoparticles were designed for COVID. But as you also mentioned, needles are a big fear of mine. So how able could these nanoparticles be designed to be any other vaccine that is not only lung disease, basically any other vaccine that you could design for the body?
BALAJI NARASIMHAN: So there are other ways of delivering vaccines without using needles. Two examples– one is a patch. So companies like 3M have designed nicotine patches that people use all the time. So you can deliver the vaccine through the skin by using patches like that. So if there are vaccines for conditions that are not necessarily affecting the lungs, you can use a patch to get this vaccine with no needles. And, of course, maybe there’s a way by which you can pop a pill that will be your vaccine, too. So those are technologies or those are approaches that our lab and other labs are working on in order to make this vaccine get to different parts of the body effectively.
IRA FLATOW: Well, speaking of that, can you use it not just for viruses but possibly anticancer things, stuff like that?
BALAJI NARASIMHAN: Yep, great question, Ira. So one of the things that these vaccines of ours do very well is they activate certain kinds of immune cells called T cells. And these T cells are a very important weapon against cancer. So if you’re looking for harnessing your own immune system to fight off that cancer, immunotherapy, which is where your T cells come in, are very important. So you can use these nanoparticle-based formulations for cancer immunotherapy.
You can also use them to deliver small amounts of drug to the brain. Current treatments for Alzheimer’s and Parkinson’s are not effective in that they only treat symptoms, and they don’t slow down the progression of disease. One of the problems is that the types of drugs you need to get into the brain require large doses of those drugs to be effective. And so by lowering the dose of the vaccine, we are able to get the vaccine or the drug to the right place at the right time, and that’s what these particles can do.
IRA FLATOW: Interesting. Yes, over here.
AUDIENCE: Would this style of vaccine be more adaptable to new variants of viruses?
BALAJI NARASIMHAN: Well, thank you for asking that wonderful question. So yes, and the reason for that is the strategy we use in designing our vaccine is we use a combination of proteins that the virus does not mutate as it evolves in our vaccine together with proteins that the virus does mutate. So the virus doesn’t change what’s inside it because the virus may believe that those are not being used to target the virus.
Alternatively, those proteins may be important for the virus to survive. So if the virus is not changing those, why don’t we teach our immune system to recognize that virus using things that it doesn’t change? And that’s what makes this approach amenable to variants.
IRA FLATOW: My last question to you is, how long until they’re available?
BALAJI NARASIMHAN: Hopefully before the next pandemic.
IRA FLATOW: Well, hope is not a policy, as they say in my business. I mean, are we talking 3 to 5 years, 10 years, what kind of–
BALAJI NARASIMHAN: Next three to five years. Three to five years is the target.
IRA FLATOW: What needs approval? Anything needs approval with the FDA or any along the way, all of that?
BALAJI NARASIMHAN: Yeah, so the process is something that the FDA would have to inspect. The quality control when we manufacture this at scale would be something the FDA would have to approve, and obviously they’d have to see data in humans. So all of these things take time. They take resources. So I’d say three to five years is a good guess, Ira, to start getting these to the point where they are translatable to the clinic.
IRA FLATOW: Interesting stuff, Balaji. Thank you for taking the time to be with us today.
BALAJI NARASIMHAN: Thank you so much today.
IRA FLATOW: Dr. Balaji Narasimhan, a distinguished professor and director of the Nanovaccine Institute at Iowa State University.
Copyright © 2024 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
D Peterschmidt is a producer, host of the podcast Universe of Art, and composes music for Science Friday’s podcasts. Their D&D character is a clumsy bard named Chip Chap Chopman.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.