A Promising New Treatment Emerges For Multiple Myeloma
13:12 minutes
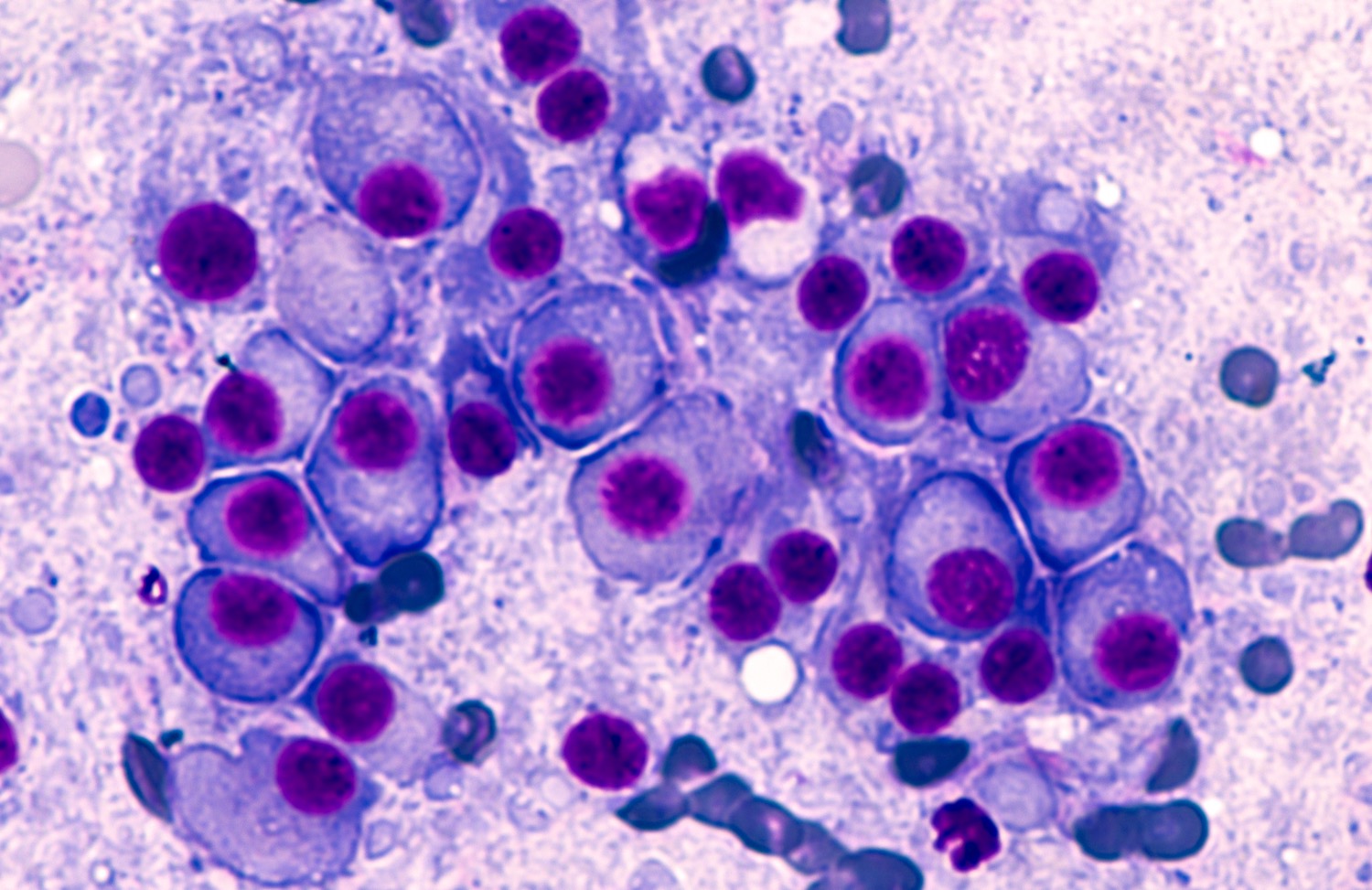
Multiple myeloma is an incurable blood cancer that affects cells inside a patient’s bone marrow. Nearly all multiple myeloma patients will relapse at some point in their treatment, becoming resistant to first one, then another frontline intervention.
But a new kind of therapy, a bispecific antibody called Talquetamab, has been showing promise in clinical trials—both in treating the cancer, and keeping patients in remission longer. A bispecific antibody works as a kind of bond between a T-cell that might otherwise not be doing its job and the myeloma cell itself, forcing the T-cell to attack the cancer.
Ira talks to Dr. Ajai Chari, who is leading the clinical trials of Talquetamab, about the historic difficulty of treating multiple myeloma, and why this new therapeutic approach may lead to more patients living longer lives.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Ajai Chari is director of clinical research for the Multiple Myeloma Program at the Mt. Sinai Icahn School of Medicine in New York, New York.
IRA FLATOW: This is Science Friday. I’m Ira Flatow.
Multiple myeloma is the second most common blood cancer in the US. And so far, it’s incurable. Patients may live years on treatments, but almost all relapse and may no longer respond to a treatment that was previously working. Researchers are looking for more effective treatments, ones that may increase the time patients are in remission or even avoid relapse entirely.
And now, a new experimental treatment is getting good numbers in clinical trials. Called talquetamab, it’s been achieving positive results in over 70% of patients overall in Phase 1 and Phase 2 clinical trials so far, and achieving remissions of months longer than existing treatment. Here to explain more, plus why multiple myeloma is such a tricky cancer to treat, is Dr. Ajai Chari, director of clinical research for multiple myeloma at Mount Sinai’s Icahn School of Medicine in New York. Welcome, Dr. Chari.
AJAI CHARI: Thank you so much, Ira. A pleasure to be here.
IRA FLATOW: Nice to have you. So you’ve gotten data from both Phase 1 and Phase 2 trials of this drug so far. What to you is the most encouraging part of the results?
AJAI CHARI: Yeah, the Phase 1 just got published in New England, and Phase 2 we just presented at our annual meeting. And I think the most exciting thing is that these are patients, some of whom have exhausted all available therapies, and we’re still seeing a response rate of 70%. And those responses occur as quickly as one month, and their deepest remissions can actually be achieved within two months.
So imagine if you’re a patient who’s exhausted all therapies to be having one of the deepest, most durable remissions you’ve had in recent years on this new therapy. So it’s incredibly gratifying for our entire health care team to be seeing these patients doing so well.
IRA FLATOW: As I mentioned, multiple myeloma is considered incurable. Why is it so common for patients to have a relapse?
AJAI CHARI: That’s the million dollar question. I guess part of it is who gets myeloma. These typically are patients in their 60s and 70s. And we think perhaps everybody might have a little bit of an abnormal plasma cell. So the culprit cell in myeloma is known as a plasma cell, which normally makes antibodies. But when this cancer becomes cancerous or malignant, rather than making all the antibodies we need to fight off infections, it overproduces one antibody.
One possible hypothesis is that, if we have small levels of these abnormal cells when we’re younger, our immune system is able to survey and get rid of them. And then perhaps that gets lazier as we get older. And there’s a lot of genetic complexity to myeloma and immunologic complexity. So between the age, the disease, the immune microenvironment, those are probably all factors as to why every treatment works for a while, but then it stops working.
IRA FLATOW: Yeah. Well, tell me then, what is there about this treatment that works so differently from existing treatments?
AJAI CHARI: It’s really remarkable. Because historically, to get a new drug approved in this, what we call, unmet need– so if you take a patient that’s exhausted all available therapies at that time– the benchmark was a 20% to 30% response rate, lasting three to four months. And now– we never thought we’d be attaining these results– but between this mode of action, called bispecifics, and a separate one called CAR-T, we’re saying 70 to 100 is the new 20 to 30. And those are the responses we’re seeing.
Even though we wouldn’t even have expected these T-cells, which are basically the sniper cells here that we’re actually activating– in these patients who’ve had up to five, six different types of chemotherapy cocktails, or lines of therapy, over, say, the last six years, in spite of having been beaten up by all of these regimens in terms of the immune system, we’re getting these outstanding responses. And it probably just speaks to this untapped potential.
A lot of our treatments have been targeting the cancer and maybe some parts of the immune microenvironment. But this really is harnessing probably one of the most important sniper cells, if you will, the T-cell. And presumably that’s a big part of why 70 to 100 is the new 20 to 30.
IRA FLATOW: Well, that’s what I’m trying to understand. What does this drug do with the T-cells that the other drugs are not doing?
AJAI CHARI: So it’s actually interesting. If we go back a little bit in medical history, every human monoclonal antibody, whether it’s for COVID, autoimmune diseases, cancers, it’s all due to myeloma. Back in the ’80s, the Nobel Prize was given to somebody who decided to fuse a myeloma cell to a spleen cell. And that fused cell, called a hybridoma, cranked out antibodies. And so you can genetically, in the laboratory, manipulate these cells and make different antibodies that we need, whether it’s to treat COVID or other things.
The first antibody for myeloma didn’t get approved until 30 years later. And that was considered a naked antibody. It has this Y-shaped structure, and the two parts of the why bind to whatever your target is– typically the myeloma. Here, the innovation is it’s a bispecific antibody. So the Y-shaped structure, one part is binding to the myeloma and the other side is binding to the T-cell, the sniper cell. So depending on what somebody is into, you can consider them handcuffs or you can consider it double-sided tape.
But basically, these T-cells that are existing within each patient are being trafficked to exactly where the cancer is. And then these T-cells come alive. They realize, hey, this is an enemy. They release chemicals. And those chemicals poke holes in the cancer membrane. And these cancer cells wither away rapidly.
So it’s a remarkable feat of accomplishment. But these bispecific antibodies– there was one approved many years ago– or several years ago– for acute lymphocytic leukemia. But it’s a rare condition and only given in academic centers. Here, these bispecific antibodies, myeloma is the first. One just got approved a few weeks ago. This one probably would be second. But there’s other diseases, including lymphomas, leukemias– this is a broad approach to treating cancer. It’s kind of a designer antibody, not just the original antibody that we’ve had for 30 years but the next generation.
IRA FLATOW: So what I hear you saying is that the drugs help the T-cells, help the immune system, find the cancer, and then attack it. Would that be right?
AJAI CHARI: Correct. Exactly.
IRA FLATOW: Because cancers usually evade the immune system. But you have found a way of getting around that.
AJAI CHARI: Yeah. And what’s particularly striking, these are in patients with a median age of 67, with many prior chemotherapies. So this is what’s so remarkable, that the 70 to 100 in such heavily treated patients. And of course, it begs the question of how might this do even in less heavily treated patients. Can we see a future where– can we put an end to chemotherapy? Because no chemotherapy drug is giving this kind of response rate as a single agent. We certainly combine drugs. And I don’t want to dismiss– we’ve made a lot of progress on the backbones of those agents, but this is potentially a logarithmic improvement in terms of outcomes.
So there’s a lot of excitement. We’re just at the cusp of this type of treatment. And this is single-agent therapy, but both combinations and in less heavily treated patients, is really exciting as well to think about the future.
IRA FLATOW: Doctor, let’s talk about the side effects. Are they manageable?
AJAI CHARI: Yes. I always think it’s important to take the patient experience, especially as we get more choices. And doctors and nurses can say one thing, but ultimately it’s the patient who votes with their feet. So the number of patients that came off this study, which was about 288 patients, was 5%. So 5% came off due to adverse events. Which is relatively low. And I think the remaining 95% stayed on treatment as long as it was benefiting them. So I think–
IRA FLATOW: That’s amazing.
AJAI CHARI: –that speaks for itself.
IRA FLATOW: That is. We’ve talked about CAR-T therapy on the show before, which is another way– and you mentioned it– to get T-cells to work more effectively. Could your bispecific antibodies be better than CAR-T and more affordable?
AJAI CHARI: So when I was asked a similar question at our national conference, my response was what I’m going to tell you now. I think these are all like our children, right? We have to love them all. And different kids have different strengths. And that’s what I would say here as well.
And one way I would translate this is I was actually assigned bispecifics as a topic recently at the European Hematology Association. And the debate was CAR-T versus bispecific. And I think the pros of CAR-T are it’s really ideally a one-and-done approach. Because there, you’re taking– a big difference is you have to take each patient’s T-cells out of the patient by a process called apheresis. It’s like a dialysis process. And then the laboratory genetically manipulates it. And then it’s put back into the patient. So it’s personalized immunotherapy, if you will. But it takes a lot longer because of the nature of having to do all of that manipulation.
In contrast, bispecifics are off the shelf. It’s the same product that every patient is getting. It’s not personalized in the way that CAR-T is. And it means it’s ready to go. And I think that’s one of the big differences. Because if you can imagine, these are patients who’ve had typically five different types of chemotherapy. They’ve exhausted all available drugs. And if your myeloma is exploding, you don’t have the time to wait for collection, manufacturing, administration.
So I think probably one of the biggest differentiating factors between the two is that patients with rapidly progressive disease don’t have the luxury of waiting for a CAR-T. They need to go to a bispecific. And also, there’s tremendous constraints right now in CAR-Ts between the so-called vectors– the viruses that are used to make CAR-T, the number of spots, lengthy wait times. So the way I would conclude it is I think both are important. Both are extraordinary developments. Both are in the 70% to 100% response rate.
But the analogy I closed with in my debate was these CAR-Ts are like Rolls-Royce Phantoms– very hard to get, we all want them, but rare and expensive. But the bispecifics, I would argue, are not that necessarily different in terms of expense. Because you’re giving the drug repeatedly. So CAR-T, you do one costly intervention. And there is some recovery period there, too. But the bispecifics have to be given typically, depending on the drug, anywhere from weekly to monthly. And so there is cost with that.
But I think the comparison would be Toyota Corollas, right– widely available, the most sold car globally, and really what makes the world go round. So bispecifics I could foresee eventually also being given in the community. I don’t see that happening with CAR-T anytime soon. Because basically, CAR-Ts are like transplants. They’re going to be done at large academic centers.
And so they’re really different products. And I think we need them all. And also, we’re so early. We’re going to probably also have sequencing issues. Just because you get one doesn’t mean you can’t get the other. But we need to generate that data too.
IRA FLATOW: Dr. Chari, I have one last question for you. Because I know, we broadcast this on the radio and podcasting it, and all the people who are ill with cancer, and especially multiple myeloma, they’re going to say, how do I get in on either one of these tests, or when can I get this drug for me? What do you say to them?
AJAI CHARI: I would say it’s very important for every myeloma patient, even from newly diagnosed all the way to those who’ve had all of the easy drugs that are approved by the FDA– it’s really important to work in collaboration with an academic myeloma center. And studies have shown that those patients who do that actually have better outcomes and live longer.
So one is to have that partnership. And it doesn’t mean you have to drive hours every day to get all your treatment, or every week. But it means there should be a collaborative relationship.
IRA FLATOW: Well, what I’m asking is, I guess, is it available? I mean, if you drive to get your stuff, is it available to drive to and get the treatment?
AJAI CHARI: I think there’s two ways– there are now two commercial CAR-Ts, and there’s also a commercial bispecific. So there’s three products that are available, but they’re not being done in the community yet. So you’d have to go to an academic medical center.
Then there’s a bunch of additional CAR-Ts and bispecifics that are actually in clinical trials. Because as I said, the CAR-T slots are few and far between, and there’s a research CAR-T slot that’s actually demonstrating activity. So that’s why I was encouraging collaboration with academia. Because right now, all of these products are very tightly linked. And there’s a steep learning curve to giving them– which has been mastered– but for now, I would say collaboration. But in the future, I would love to see these patients getting their bispecifics from their community oncologists. But I think that’s going to take at least six months to a year to get all of those kinks worked out.
IRA FLATOW: OK, I got a number out of you. Because that’s what everybody wants to know is how long is it going to be till the average person in the public can get it.
AJAI CHARI: It is available now in all the academic centers. Because the first bispecific just got approved, and we’re all trying to launch those. So contact your closest academic myeloma center.
IRA FLATOW: Well, that’s good news.
AJAI CHARI: Yeah.
IRA FLATOW: Dr. Chari, thank you for taking time to be with us today.
AJAI CHARI: Thank you so much for having me.
IRA FLATOW: Dr. Ajai Chari, director of clinical research for multiple myeloma at Mount Sinai’s Icahn School of Medicine in New York.
This is Science Friday, from WNYC Studios.
Copyright © 2022 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/.
Christie Taylor was a producer for Science Friday. Her days involved diligent research, too many phone calls for an introvert, and asking scientists if they have any audio of that narwhal heartbeat.
Ira Flatow is the founder and host of Science Friday. His green thumb has revived many an office plant at death’s door.