Fighting Cancer With Your Own Immune System
12:14 minutes
Just months ago, former president Jimmy Carter announced that he had melanoma and that this particular form had spread to his brain. On Sunday, the 91-year-old made a shocking announcement about his health: He was cancer-free. Speaking before his church in Georgia, he stated, “I’ve been treated for my cancer with a new medicine that was developed just in the last few years.” That new medicine is pembrolizumab, a cancer immunotherapy drug that is commercially known as Keytruda. Doctors Antoni Ribas and Padmanee Sharma, who work on immunotherapy treatments for cancer at UCLA and MD Anderson Cancer Center, respectively, join Ira to talk about how the immune system can be trained to fight cancer, and where the research is heading.
Antoni Ribas is a professor of medicine and the director of the Tumor Immunology Program at the University of California, Los Angeles, in Los Angeles, California.
Padmanee Sharma is the scientific director of the Immunotherapy Platform at MD Anderson Cancer Center in Houston, Texas.
IRA FLATOW: This is Science Friday. I am Ira Flatow. At 90, former President Jimmy Carter’s cancer diagnosis seemed dire. At the end of the summer he announced that the form of melanoma he had had spread to his brain. And now, just a few months later, at the age of 91, Carter made a big announcement. Standing before his Sunday school class in Georgia this past week, he revealed that his most recent MRI brain scan revealed no detectable traces of cancer.
JIMMY CARTER: I’ve been treated for my cancer with a new medicine that was developed just in the last few years.
IRA FLATOW: That new medicine? A cancer immunotherapy drug. Joining me now to discuss how doctors are working to train your immune system to fight cancer are my guests, Padmanee Sharma, she is Scientific Director of the Immunotherapy Platform at M.D. Anderson Cancer Center in Houston, Texas. Welcome to Science Friday.
PADMANEE SHARMA: Thank you.
IRA FLATOW: Antoni Ribas is a Professor of Medicine and Director of a tumor immunology program, University of California at Los Angeles in. California. Antoni, welcome to Science Friday.
ANTONI RIBAS: Good afternoon. Hello.
IRA FLATOW: Let’s talk about what is cancer immunotherapy Antoni? What is the drug that was used, and what do we mean by that?
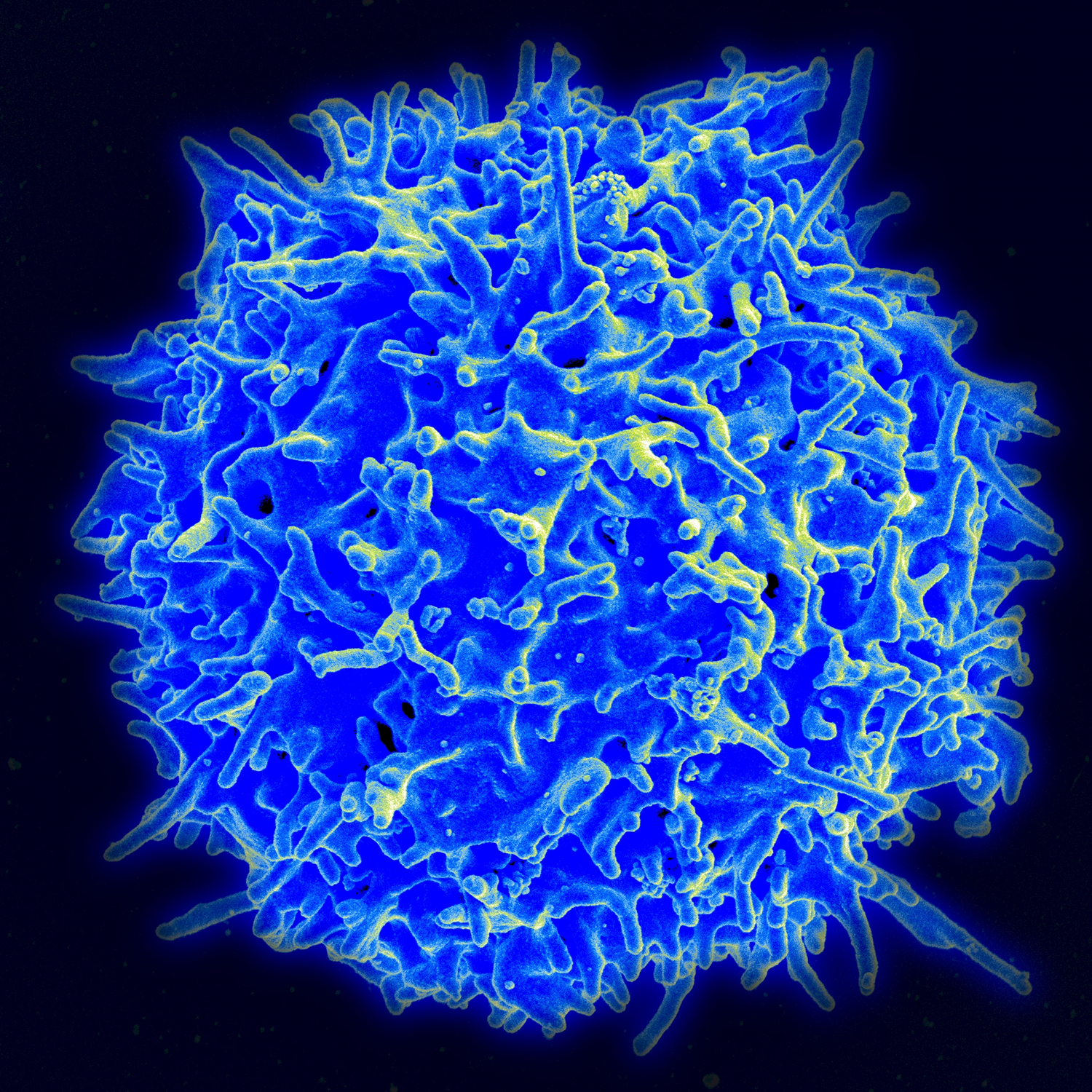
ANTONI RIBAS: The idea is to use the patient’s own immune system to attack the cancer, which has been a centuries-old idea that has been tried in many ways. But the way it’s working with this new class of drugs is by releasing brakes to the immune system where the immune system is trying to attack the cancer. The cancer is hiding from it, and then we take away what allows the cancer to hide.
IRA FLATOW: What exactly does the cancer use to hide?
ANTONI RIBAS: Whenever the immune system cells infiltrate the tumor, the cancer makes a kind of a shield by a protein called PD-L1. And what we do is block that, and then the cancer cannot hide, and the immune system attacks the cancer.
IRA FLATOW: Is this something relatively new?
ANTONI RIBAS: It is. The concept comes from around 15 years ago when Dr. Jim Allison who is the colleague of Pam Sharma, developed this idea that maybe we were wrong for a 100 years trying to turn on the immune system with vaccines and things like these when we’re dealing with cancer. That what we needed to do was to release its brakes.
IRA FLATOW: And so, you basically are training the immune system to find the cancer?
ANTONI RIBAS: Yes. The immune system is designed to fight bacteria and viruses, things that come from outside. But when it’s trying to attack something from the inside, then it has a series of checks and balances that doesn’t allow the immune system to work against the cancer. And the cancer hides behind that. Now, with this new class of agents, it cannot hide anymore, at least in the patients where this works.
IRA FLATOW: So Dr. Sharma, what we’re saying is that we’ve taken the defense mechanism, the hiding mechanism, away from the cancer cells so that our own body can attack it normally.
PADMANEE SHARMA: Yes. I mean, just to expand a little bit more on this idea, the immune system is very, very powerful. The immune system is what keeps you protected from viral and bacterial antigens as Toni just mentioned. But the other important thing is that the immune system has many off switches, so that not only does the immune system get turned on, but my immune system, your immune system, everyone’s immune system has these off switches.
So it’s not just in the cancer patients. The off switches are important, because the off switches make sure that the immune system does not take off and create autoimmune diseases, for example. So the off switches are very important. But what Jim Allison’s group showed, that if you block these off switches, you allow the immune system to go for longer periods of time, which is what is necessary to allow for tumor rejection in cancer patients.
And so, understanding the basic immunology, and understanding about these off switches– the first was CTLA-4, and now the second is the PD-1, PD-L1, these off switches, when we block them, allow us then to have a powerful immune response against cancer in some patients.
IRA FLATOW: A lot of people have been reporting that President Carter was cured. He’s not officially cured, is he?
PADMANEE SHARMA: It would take time for us to follow him and do repeat imaging studies to look and make sure that the cancer is not recurring. But cure is the word we would like to be able to use after we see repeated imaging studies that do not show the cancer coming back.
IRA FLATOW: Why, in the studies, are only about 30% of the people having as good a result is the President did?
PADMANEE SHARMA: So some of that has to do with the fact that there are multiple different off switches. So the drug that President Carter received blocks one of those off switches, but there are many, many other off switches. And so, these off switches, we need to understand which tumor types they’re playing a role in and which patient they’re playing a role in so that we can block the appropriate off switches, and maybe need to block multiple off switches so that we allow the immune response to take off and do the job in more patients.
IRA FLATOW: Could the fact be that he is living past where most of us live and is in his 90s, and therefore, maybe has a great immune system to begin with, and that when you tweak it up it gets even better?
PADMANEE SHARMA: So we’ve seen these types of responses in both younger and older patients. And then, actually what you’re saying is opposite to what most people say because people say as you get older your immune system is not as good. And so, they think that these kind of responses are more seen in younger patients. Actually, we’ve seen these types of responses in both younger and older patients. It seems that we can create an anti tumor immune response in all different age groups.
IRA FLATOW: Ribas, what kind of the side effects, Antoni, are we going to see with this? Or there are no really side effects?
ANTONI RIBAS: So as Pam was saying, these off switches are not there for us to treat cancer. They’re there because the immune system, when unleashed, can attack normal organs. But this particular one seems to be very specific for the immune system cells that were trying to attack the cancer. And whenever we release it, the side effects are really low.
It’s not chemotherapy. So it does not make the hair fall, it does not give nausea or vomiting. It’s not the regular cancer treatment. In some patients it can unleash an immune response against normal organs, and it will induce these diseases where the immune system attacks normal tissues, which is autoimmunity. But with this particular one, pembrolizumab, Keytruda, and a similar one that’s called nivolumab of Opdivo, it’s in around 1 in 10 patients would have that kind of side effect.
IRA FLATOW: Wow. Dr. Sharma , do you think it’s possible, we always ask this question, that this kind of treatment can treat all cancers at some point with this type of therapy, even though it’s currently only FDA approved for three types?
PADMANEE SHARMA: So first of all, it’s an amazing thing that we’ve reached, right? This is an amazing time in cancer therapy because we now have immunotherapies that are working in multiple tumor types, working in melanoma, kidney cancer, and lung cancer. So what I wanted to say was we never even thought that was possible that you can take one type of drug and basically have it work across all these different tumor types.
And so the important point is that you’re blocking an inhibitory pathway, or an off switch, on T cells, which is the soldier of the immune system. And so, these T cells are the same in my body, your body, and every cancer patient. So it’s not about the tumor type per se. It’s about the fact that the T cells have these particular off switches. And so, we think we can figure out how T cells function and what the off switches so that we can use it across all the different tumor types.
Now again, you may need to use combination strategies for some tumor types; whereas, other tumor types you can use a single agent drug. But we think that we will come up with immunotherapy strategies to treat many, many different tumor types.
IRA FLATOW: Once this drug does the alert the T cells to fight the cancer, are they good forever? Do you have to keep giving the drug now that the immune system knows what it should be looking for?
PADMANEE SHARMA: Well, that again, is the beautiful thing, because when you’re treating the immune system, which is what these drugs are doing, you’re allowing then for a memory response. If you think about it, when you get the polio vaccine, or you get the smallpox vaccine, or any kind of these vaccines that you get in your childhood– they allow you to have these type of memory responses. Whereas, later on in life, if you encounter the antigen, you have these memory responses that can eliminate the antigen before you actually develop the disease.
And it’s the same thing here. These drugs are treating the immune response. And so, when you stop the drug, the immune responses still evolve to hopefully give you this memory response that can then treat the cancer if it does show up again, and treat it before it becomes a real problem for the patient. So we think it’s these type of memory responses that are allowing us to see these 10 year or more survival of patients.
And so, we’re hopeful that that’s what will allow us to use the word cure. This is very different from when we did chemotherapy or radiation therapy, because those are targeting the tumor cells, not the immune response. And so, when you stop the drug, the response is gone. But here, when you stop the drug, the immune system still survives. And that is what gives you that memory.
IRA FLATOW: And it could be still mopping up other cells that are floating around?
PADMANEE SHARMA: Absolutely.
IRA FLATOW: Wow. Wow. Dr. Ribas, where would you go from here? Where’s the next step on this?
ANTONI RIBAS: So this step has been real important, to know that a series of cancers can be treated by unleashing the immune system and attacking the tumor specifically. Obviously, the next step is to understand how it happens, and why does it work and some patients and on does not working in many others. And by studying that, then it allow us to think of what’s missing in the patients where this is not working. And how do we develop a combination therapy that could treat those other patients?
IRA FLATOW: So you can’t be really happy until you can figure how to pull in the other 2/3 of the patients that didn’t really respond as well.
ANTONI RIBAS: Absolutely. What this is doing, it’s increasing my level of expectations of the treatment. I think that every patient should be able to get this benefit. And if we don’t achieve it, it is because we have missed something. But it’s been a long process of translating knowledge from basic immunology and basic biology into these treatments. It’s a big accomplishment of advance of science and giving benefits to patients, including President Carter.
IRA FLATOW: Dr. Sharma, you agree?
PADMANEE SHARMA: I absolutely agree. I think the next step for us now is to look at large numbers of patients that we are able to give benefit to, understand how they were able to achieve the benefit, and then do the same thing, or understand what are the mechanisms preventing that benefit from the other 2/3 of patients as you mentioned, and make sure we can release the other brakes that may be coming into the play, or bringing in the other cells that are necessary, not just the T cells, to allow us to then have all of these patients having a clinical benefit. We want to make cancer something of the past.
IRA FLATOW: Well, it’s hard not to get excited about this. So we try not to. But it’s amazing results. Thank you both for taking time to explain this all to us.
ANTONI RIBAS: Thank you very much Ira.
PADMANEE SHARMA: Thank you. Padmanee Sharma Scientific Director of Immunotherapy Platform at M.D. Anderson Cancer Center, and that’s in Houston. And Antoni Ribas is Professor of Medicine and Director of the tumor immunology program at UCLA. That’s in California. We’re going to take a break, come back and look at some crazy wonderful photos from New Horizons’ closeup of Pluto Amazing stuff after the break. Stay with us.
Copyright © 2015 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of ScienceFriday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our polices pages at http://www.sciencefriday.com/about/policies.
Becky Fogel is a newscast host and producer at Texas Standard, a daily news show broadcast by KUT in Austin, Texas. She was formerly Science Friday’s production assistant.